(Diabetes Mellitus Type 2; Insulin-Resistant Diabetes; Diabetes, Type 2)
Type 2 diabetes – Definition
Diabetes is a higher level of glucose in the blood than is normal. Glucose comes from the breakdown of the food you eat. It travels through your body in the blood. A hormone called insulin then helps glucose move from your blood to your cells. Once glucose is in your cells it can be used for energy. A problem making or using insulin means glucose can not move into your cells. Instead the glucose will build up in your blood.
In type 2 diabetes, the body is resistant to high levels of insulin. This means there is plenty of insulin in the body, but the cells are unable to use it. This will lead to the build up of glucose in the blood, also called hyperglycemia. At the same time, your cells are not getting glucose they need to function well. Over a long period of time high blood glucose levels can damage vital organs. The kidneys, eyes, and nerves are most commonly affected organs.
Type 2 diabetes – Causes
Two conditions contribute to hyperglycemia in type 2 diabetes:
- Insulin resistance related to excess body fat
- Body’s failure to make an adequate amount of insulin
Type 2 diabetes – Risk Factors
Factors that increase your chance for type 2 diabetes include:
- Having a family history of type 2 diabetes
- Being obese or overweight, especially excess weight in the upper body and abdomen
- Eating a lot of meat, especially processed meat (eg, processed luncheon meats, hot dogs, sausages)
- Having cholesterol problems especially low HDL (good) cholesterol and high triglycerides
- Having high blood pressure
- Having a history of cardiovascular disease
- Having depression
- Having a history of gestational diabetes or having a baby that weighs over nine pounds
- Having an endocrine disorder (eg, Cushing’s syndrome, hyperthyroidism, acromegaly, polycystic ovary syndrome, pheochromocytoma, glucagonoma)
- Having a condition associated with insulin resistance (eg, acanthosis nigricans)
- Having previous blood test results that show impaired glucose tolerance and impaired fasting glucose
- Taking certain medicines (eg, pentamidine, nicotinic acid, glucocorticoids, thiazides)
- Having a sedentary lifestyle
- Having sleep difficulties
- Having a low birth weight
- Gender: more common in older women than men
- Race: African American, Hispanic, Native American, Hispanic American, Asian American, or Pacific Islander
- Age: 45 years or older and younger people who are obese and belong to at risk ethnic groups
Type 2 diabetes – Symptoms
You may have diabetes for years before you have symptoms you notice. Symptoms due to high blood sugar or diabetic complications may include:
- Increased urination
- Extreme thirst
- Hunger
- Fatigue
- Blurry vision
- Irritability
- Frequent or recurring infections
- Poor wound healing
- Angina
- Painful leg cramps when walking
- Numbness or tingling in the hands or feet
- In women: frequent vaginal yeast infections and urinary tract infections
- Problems with gums
- Itching
- Impotence
Type 2 diabetes – Diagnosis
The doctor will ask about your symptoms and medical history. You will also be asked about your family history. A physical exam will be done.
Diagnosis is based on the results of blood testing. American Diabetes Association (ADA) guidelines for diagnosis include:
- Symptoms of diabetes and a random blood test with a blood sugar level greater than or equal to 200 mg/dL [11.1 mmol/L]
- Fasting blood sugar test — done after you have not eaten for eight or more hours — showing blood sugar levels greater than or equal to 126 mg/dL (7.0 mmol/L) on two different days
- Glucose tolerance test — measuring blood sugar two hours after you consume glucose — showing glucose levels greater than or equal to 200 mg/dL (11.1 mmol/L)
- HbA1c level of 6.5% or higher — indicates poor blood sugar control over the past 2-4 months
mg/dL=milligrams per deciliter of blood; mmol/L=millimole per liter of blood
Type 2 diabetes – Treatment
Treatment aims to:
- Maintain blood sugar at levels as close to normal as possible
- Preventing or delaying complications (regular medical care is important for this)
- Control other conditions that you may have, like high blood pressure and high cholesterol
Diet
- Follow a balanced meal plan. Practice good portion control.
- Do not skip meals. Plan your meals and snacks through the day. Having meals regularly throughout the day can help maintain blood glucose.
- Eat plenty of vegetables and fiber.
- Eat limited amounts of fat.
- Eat moderate amounts of protein and low-fat dairy products.
- Carefully limit foods containing high concentrated sugar.
- Keep a record of your food intake. This will help a dietitian or doctor advise you.
Weight Loss
If you are overweight, talk to your doctor about a healthy weight goal. Your body will respond better to insulin after weight loss. You and your doctor or nutritionist can develop a safe nutrition plan for you.
These options may help you lose weight:
- Using a portion control plate BE
- Using a prepared meal plan
- Consider using a Mediterranean-style diet
Group education may help you with your weight loss goals.
Exercise
Physical activity plays an important role in blood glucose control. Activity can
- Make the body more sensitive to insulin
- Help you reach and maintain a healthy weight
- Lower the levels of fat in your blood
Aerobic exercise and strength training can also help to improve long term glucose control (HbA1c levels). Regular exercise can also help reduce your risk of heart disease.
Talk to your doctor about an activity plan and any precautions you should take.
Oral Medication
Certain medicine will help you manage your blood glucose.
Your doctor may recommend medicine taken by mouth such as:
- Metformin — help to reduces the amount of glucose made by the body and also makes the body more sensitive to insulin
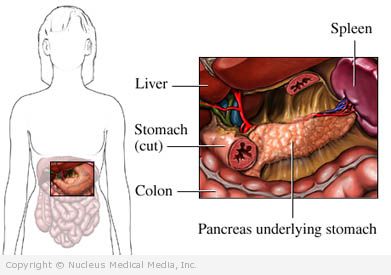
- Drugs that prompt the pancreas to make more insulin (eg, sulfonylureas [ glyburide, tolazamide ], dipeptidyl peptidase-4 inhibitors [ saxagliptin, sitagliptin ], and repaglinide [Prandin], linagliptin [Tradjenta])
- The FDA has warned that sitagliptin may increase the risk of acute pancreatitis.
- Insulin sensitizers — help the body better use insulin such as, pioglitazone
- Starch blockers — decrease the amount of glucose absorbed into the blood such as acarbose or miglitol)
Some medicine needs to be given through injections such as:
- Incretin-mimetics such as, exenatide — which stimulate the pancreas to produce insulin and suppress appetite — often leading to weight loss
- Amylin analogues such as pramlintide — which replaces a protein that is normally produced by the pancreas that is low in people with type 2 diabetes
Insulin
For some, the body does not make enough insulin. Insulin injections may be needed. It may be used if blood sugar levels can not be controlled with lifestyle change and medicine.
Blood Sugar Testing
Checking blood sugar levels during the day can help you stay on track. It will also helps your doctor determine if your treatment is working. Testing is easy with a monitor. Keeping track of blood sugar levels is especially important if you take insulin. Frequency of testing is determined by how well your blood sugar control is doing.
The HbA1c may also be done at your doctor’s office. Doctors advise that most keep their HbA1c levels below 7% (ADA recommendation). This level has been shown to lead to fewer diabetic complications.
Regular blood sugar testing may not be needed in patients with type 2 diabetes. It may not be needed for those whose condition is under reasonably good control without insulin. Talk with your doctor before stopping blood sugar monitoring.
Alternative Therapies
One study focused on people with a specific type 2 diabetes. When given vitamin E, they showed a decrease in the rates of heart problems.
Type 2 diabetes – Prevention
Lifestyle changes seem to be most effective. To reduce your chances of developing type 2 diabetes:
- Participate in regular physical activity.
- Maintain a healthy weight.
- Drink alcohol in moderation (two drinks per day for a man, and one drink per day for a woman)
- Eat a well-balanced diet:
- Get enough fiber
- Avoid fatty foods
- Limit sugar intake
- Eat more green, leafy vegetables
BE = This therapy has the best evidence available showing that it is effective.