Heartburn – Overview
(Gastroesophageal Reflux Disease; Gastro-oesophageal Reflux Disease [GORD]; GERD; Reflux, Heartburn)
Heartburn – Definition
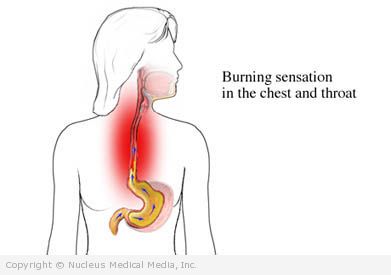
Heartburn is a burning sensation in the lower chest. It is the main symptom of gastroesophageal reflux disease (GERD).
Heartburn – Causes
When you eat, food travels down the esophagus to the stomach. The muscle between the esophagus and stomach lets food enter the stomach. When this muscle weakens, stomach acid flows into the esophagus. This causes a burning sensation, called heartburn.
Other causes of GERD include conditions that:
- Interfere with food passing through the esophagus
- Cause excess acid production
Genetics may also play a role in developing GERD.
Heartburn – Risk Factors
Risk factors include:
- Being obese
- Being pregnant
- Having a hiatal hernia — a weakening in the diaphragm (large muscle separating the thorax and the abdomen) causing the stomach to partially slip into the chest cavity
- Exercising immediately after eating (especially jogging or running)
- Smoking
- Using alcohol
- Eating chocolate (can worsen symptoms)
- Drinking caffeinated beverages
- Eating a high-fat diet
- Taking certain medicines, including:
- Anticholinergics
- Calcium channel blocking agents
- Theophylline
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Quinidine
- Tetracycline
- Potassium and iron supplements
- Anti- osteoporosis agent alendronate
- Hormone replacement therapy
- Having prior surgery for heartburn, including gastric reflux surgery and vagotomy
- Having asthma and using asthma medicines
- Having and treating a peptic ulcer
- Having certain conditions, including diabetes, cancer, scoliosis, cystic fibrosis, and nervous system diseases
- Having defects in the respiratory system or gastrointestinal (GI) system
- Having food allergies
Heartburn – Symptoms
Heartburn symptoms usually occur after overeating or lying down after a big meal. The symptoms may last for a few minutes or a few hours.
The severity of symptoms depends on the:
- Reason the muscle is weakened
- Amount of acid entering the esophagus
- Amount of saliva to neutralize the acid
Symptoms include:
- Burning feeling that starts in the lower chest and moves up the throat
- Feeling that food is coming back up
- Sour or bitter taste in the throat
- Pain that increases when bending over, lying down, exercising, or lifting heavy objects
Other symptoms and complications of reflux include:
- Sore throat
- Hoarseness
- Chronic cough
- Feeling of a lump in the throat
- Asthma
- Hoarse voice (laryngitis)
- Waking up with a sensation of choking
If reflux persists, the acid can damage the esophagus. Symptoms of esophageal damage include:
- Bleeding and ulcers in the esophagus
- Difficulty swallowing
- Vomiting blood
- Black or tarry stools
- Inflammation and scarring of the esophagus
- Barrett’s esophagus — This is a precancerous condition of the esophagus that has no unique symptoms. However, it can be diagnosed by endoscopic exams.
- Dental problems (due to the effect of the stomach acid on the tooth’s enamel)
When Should I Call My Doctor?
It is common to experience heartburn occasionally. But, if you have frequent episodes of heartburn (like twice a week), make an appointment to see your doctor. Also, call your doctor if you have any symptoms that are listed as complications of reflux, especially symptoms of esophageal damage.
When Should I Call for Medical Help Immediately?
Heartburn and chest pain due to a heart attack can feel similar. Get medical help right away if you have:
- Squeezing or chest pressure
- Pain in the left shoulder, left arm, or jaw
- Trouble breathing
- Sweating, clammy skin
- Nausea
- Weakness
- Lightheadedness or dizziness
- Pain that starts during activity or stress
If you are not sure of the cause of any pain in your chest, call for emergency help right away.
Heartburn – Diagnosis
The doctor will ask about your symptoms and medical history, and perform a physical exam. Tests may include:
- Upper GI series — a series of x-rays of the upper digestive system taken after drinking a barium solution
- 24-hour pH monitoring — a probe placed in the esophagus tracks of the level of acidity in the lower esophagus
- Manometry — a test that measures muscle pressure in the lower esophagus
- Endoscopy — a thin, lighted tube is passed down the throat to look at the esophagus and stomach, a tissue sample may be taken
- Biopsy — a small sample of esophageal tissue is removed to measure the amount of acid or pressure in the esophagus
Heartburn – Treatment
Treatment aims to decrease the number of episodes of heartburn and its complications. This focuses on:
- Stopping the flow of acid back into the esophagus
- Decreasing production of stomach acid
Treatment may include:
Lifestyle Changes
Lifestyle changes may include:
- Keep a food diary of what you eat and what the reaction is. Make gradual changes to your diet and record the results.
- Avoid foods that may cause symptoms, such as:
- High-fat foods
- Fried foods
- Spicy foods
- Onions and garlic
- Chocolate
- Peppermint
- Citrus fruits
- Tomatoes
- Peppers
- Alcohol
- Coffee
- Carbonated drinks
- Eat smaller portions.
- Allow at least 2-3 hours between meals and lying down.
- Lose weight.
- If you smoke, quit.
- Avoid belts and clothing that are too tight. This may increase pressure on the abdomen.
- Elevate head of bed 6-8 inches.
Medication
Medicines may include:
- Proton-pump inhibitors BE — to suppress acid production or reduce the chance of acid entering the esophagus (eg, omeprazole, lansoprazole)
- Over-the-counter antacids — to neutralize stomach acid; works quickly, but can cause problems with long-term use (eg, Maalox Advanced Regular Strength, Tums, Rolaids, Mylanta)
- Over-the-counter H2-blocker drugs — to stop the stomach from producing as much acid (eg, cimetidine, famotidine, ranitidine)
- Medicines that coat and protect the lining of the stomach (eg, sucralfate)
- Medicines that improve muscle tone in the lower esophageal sphincter (eg, metoclopramide)
Procedures
If symptoms are severe and you cannot tolerate the medicines, surgery may be an option.
The most common surgery for heartburn is fundoplication. The doctor wraps the stomach around the esophagus. This creates pressure on the muscle at the opening to the stomach. If you have a hiatal hernia, it can also be repaired at this time.
In some cases, the surgery can be done with smaller incisions, called laparoscopy.
Endoscopic Procedures
An advantage of endoscopic techniques is that they do not involve incisions in the skin. Instead, the doctor inserts a lighted device called an endoscope through the mouth and down the esophagus to reach the first part of the stomach. Through the endoscope, the doctor can perform one of a variety of procedures that decreases the backward flow of stomach acid into the esophagus, including transoral incisionless fundoplication (TIF).
If surgery or endoscopy is successful, you may not need to take heartburn medicines anymore.
Heartburn – Prevention
Lifestyle changes can help prevent heartburn, including:
- Avoid overeating.
- Sit up for 2-3 hours after eating.
- Avoid wearing tight clothing.
- Elevate the head of your bed.
- Do not smoke.
- Avoid drinking beverages that contain alcohol or caffeine.
- Change your diet to avoid certain foods.
- Chew sugarless gum for about 30 minutes after a meal. This will increase saliva flow, which can neutralize stomach acids in the esophagus.
- Maintain a healthy weight.
- Manage stress.
BE = This therapy has the best evidence available showing that it is effective.