(Insulin Dependent Diabetes Mellitus; Juvenile-Onset Diabetes; Ketosis-Prone Diabetes; “Brittle” Diabetes; Diabetes Mellitus Type 1; Diabetes, Type 1)
Type 1 diabetes – Definition
Diabetes is a higher level of glucose in the blood than is normal. Glucose travels through your body in the blood. A hormone called insulin then helps glucose move from your blood to your cells. Once glucose is in your cells it can be used for energy. A problem making or using insulin means glucose can not move into your cells. Instead the glucose will build up in your blood.
In type 1 diabetes, the body does not make enough insulin. This will lead to the build up of glucose in the blood, also called hyperglycemia. At the same time, your cells are not getting glucose they need to function well. Over a long period of time high blood glucose levels can damage vital organs. The blood vessels, heart, kidneys, eyes, and nerves are most commonly affected organs.
Type 1 diabetes is often found during childhood and young adulthood.
Type 1 diabetes – Causes
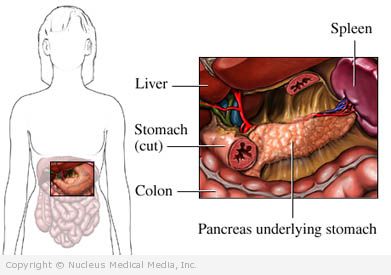
Our immune system keeps us well by fighting off and destroying viruses and bacteria. Unfortunately, sometimes the immune system attacks healthy tissue. Most type 1 diabetes develop because the immune system attacks and destroys the cells that make insulin. These cells are in the pancreas.
It is not yet clear why the immune system attacks these cells. It is believed that some people have genes that make them prone to getting diabetes. For these people, certain triggers in the environment may make the immune system attack the pancreas. The triggers are not known but may be certain viruses, foods, or chemicals.
Type 1 diabetes – Risk Factors
Risk factors include:
- Family history (parent, sibling) of type 1 diabetes
- Age: starts at age 4 with peak at ages 11-13
- Sex: more common in males than females
- Ethnicity: Northern European, Mediterranean, African Americans, Hispanics
- Increased age of mother during pregnancy
- Risk increases with increase in birth weight
- Obesity during childhood
- Other autoimmune illness, including:
- Hashimoto’s disease — disease of thyroid
- Graves’ disease — disease of thyroid
- Addison’s disease — disorder of the adrenal glands
- Pernicious anemia
- Celiac disease — autoimmune disease of the digestive tract
- Vitiligo — disorder that affects the skin cells
Type 1 diabetes – Symptoms
If you have any of these symptoms, do not assume it is due to type 1 diabetes. These symptoms may be caused by other conditions. Tell your doctor if you have any of these:
- Weight loss
- Increased urination
- Extreme thirst
- Hunger
- Fatigue, weakness
- Blurry vision
- Irritability
- Headaches
Without insulin your body will need to find new forms of energy. This will cause an imbalance in the body called ketoacidosis. It is a severe state that can lead to coma or death. Symptoms of ketoacidosis include:
- Vomiting and nausea
- Abdominal pain
- Dehydration (not enough fluid in the body)
- Drowsiness
- Abnormally deep and fast breathing
- Coma
- Dry skin and mouth
- Fruity breath odor
- Rapid pulse
- Low blood pressure
Type 1 diabetes – Diagnosis
The doctor will ask about your symptoms. You will also be asked about your medical and family history. A physical exam will be done.
Type 1 diabetes is diagnosed based on the results of blood tests and other criteria. These include:
- Symptoms common with diabetes and a random blood test showing a blood sugar level greater than or equal to 200 mg/dL* (11.1 mmol/L)
- Fasting blood test showing blood glucose levels greater than or equal to 126 mg/dL (7.0 mmol/L) on two different days — test is done after you have not eaten for eight or more hours
- Glucose tolerance test results with blood glucose greater than or equal to 200 mg/dL (11.1 mmol/L) — test is done after you eat glucose
- HbA1c level of 6.5% or higher — measure of blood sugar over the past 2-4 months
*mg/dL = milligrams per deciliter of blood, mmol/L = millimole per liter of blood
You may also need other blood tests to confirm diabetes is type 1 and not type 2. These may include:
- C-peptide tests — to see how much insulin is being made by the pancreas
- Tests that look for antibodies that are working against your pancreas
Type 1 diabetes – Treatment
Diabetes treatment goal is to maintain blood sugar at levels as close to normal as possible. Regular medical care is important for preventing or delaying complications.
Insulin
Insulin injections replace the insulin you are missing. The amount given is based on a blood glucose test you take before and after meals and at bedtime. You will need to have insulin shots two or more times daily.
You may also have an insulin pump that automatically gives you small amounts of insulin through the day.
Pramlintide
Amylin is made in the pancreas along with insulin. In people with type 1 diabetes, this hormone like insulin is missing. The missing amylin may be responsible for the blood glucose rise after a meal in people with diabetes. The drug pramlintide (Symlin) may be used when insulin therapy is not enough to control blood sugar.
Type 1 diabetes – Diet
If you have type 1 diabetes, you should meet often with a registered dietitian. Generally speaking, it is best to:
- Follow a well-balanced meal plan with a variety of food groups.
- Eat at regular times each day. Include a bedtime snack in your meal plans. Do not skip meals
- Avoid highly refined carbohydrates. This includes sugar or high fructose products like soda.
Exercise
Exercise is encouraged as long as blood glucose levels are under control. Follow your doctor’s advice on activity levels and changes you may need to make.
You may need to adjust your insulin dose or diet if you are having low glucose levels after exercise.
Type 1 diabetes – Blood Sugar Testing
Regular blood glucose checks throughout the day will help you manage your diabetes. Testing is often done with a blood glucose monitor. You can also ask your doctor about continuous monitoring systems that you wear all day.
Keep a record of the results to show your doctor. Your treatment plan may change based on your test results. The HbA1c blood test is also used by your doctor to assess your overall glucose control.
Pancreatic Islet Cell Transplant
This is a procedure that is still being investigated. It involves transplanting islet cells from a donor to a person with type 1 diabetes. After the transplant, these new cells are able to produce insulin. In some cases, people who receive these transplants may no longer need insulin injections.
Closed-Loop Artificial Pancreas
This device is still being studied. It is a continuous glucose monitoring system (CGMS). This system can automatically checks glucose levels through the day. Insulin is then delivered as needed through the day and night. The monitoring system will allow you to keep your blood sugar levels within the normal range without daily testing or injections.
Pancreatic Transplant
A pancreatic transplant may be recommended if you have:
- Severe kidney disease that requires a kidney transplant
- Acute diabetic complications or emergencies that can not be prevented by insulin
- Severe problems due to injecting large amounts of insulin
- Severe and frequent complications related to diabetes
If you are diagnosed with type 1 diabetes, follow your doctor’s instructions.
Type 1 diabetes – Prevention
Currently, there is no known way to prevent type 1 diabetes.
Some research is looking at the effectiveness of suppressing the immune system. This may be helpful in people who are at high risk of developing type 1 diabetes.