Trigeminal Neuralgia
(Tic Doleureux)
Trigeminal neuralgia – Definition
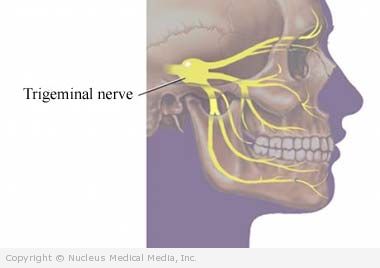
Trigeminal neuralgia (TN) is a disorder of the trigeminal nerve (fifth cranial nerve) that causes severe, shooting pain along one side of the face. The trigeminal nerve senses touch, pain, pressure, and temperature. It also helps make saliva and tears.
In TN, pain usually lasts for less than a second to a few seconds and may come and go for days, weeks, months, or years. It may go into remission or stop completely for months or years. Over time, though, the attacks may become more frequent and more severe. Attacks can be brought on by chewing, washing, shaving, touching, or even a breeze on the face.
Trigeminal neuralgia – Causes
In most cases, the cause is unknown. In some cases an abnormally formed artery or vein near the nerve is the culprit. The blood vessel can compress the nerve and cause problems. Rarely, TN may occur as a symptom of another underlying disorder, such as:
- Tumor in the brain or head
- Multiple sclerosis
- Shingles
Trigeminal neuralgia – Risk Factors
These factors increase your chance of developing TN. Tell your doctor if you have any of these risk factors:
- Age: 50 or older
- Sex: female
- Certain conditions (eg, multiple sclerosis, high blood pressure)
Trigeminal neuralgia – Symptoms
The main symptom is searing pain on one side of the face. The pain may be felt inside the mouth or in the lips, cheek, chin, nostril, ear, or near the eye. Rarely, pain may occur in the eye or forehead. Twitching or wincing sometimes accompanies the pain.
The pain is typically sudden, severe, and stabbing. Even though the pain is often brief (less than two minutes) it can reoccur hundreds of times per day. Attacks can become totally disabling. They may seem to occur at random or be triggered by extremes of temperature, washing, shaving, touching, or tickling the face. There are usually no symptoms between attacks, except perhaps a dull ache.
Trigeminal neuralgia – Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done.
Tests may be done to help diagnosis underlying conditions that may lead to TN. These may include:
- CT scan — a type of x-ray that uses a computer to make pictures of structures inside the head
- MRI scan — a test that uses magnetic waves to make pictures of structures inside the head
You may be given the antiseizure medication (eg, carbamazepine). This medicine may reduce pain and is sometimes used to help diagnose the disorder.
Trigeminal neuralgia – Treatment
Treatment usually begins with medicine. If medicine fails, other options are available.
Medications
Medicines may include:
- Carbamazepine
- Other antiseizure medicines (eg, phenytoin, gabapentin, lamotrigine, oxcarbazepine, pregabalin, topiramate)
- Low-dose antidepressants (eg, amitriptyline, clomipramine)
- Muscle relaxer (eg, baclofen)
- Other medicines, such as sumatriptan (Imitrex) injection, lidocaine nasal spray, pimozide (Orap)
Surgery
Surgical options include:
- Surgery to remove an artery or tumor that is pressing on the nerve
- Surgery to cut the trigeminal nerve
Surgery can be highly effective in some cases. The most common procedure is microvascular decompression.
Other Treatments
These procedures may be somewhat less effective than microvascular surgical decompression. But, they are widely used, especially in older patients.
- Stereotactic radiosurgery
- Injections of alcohol or glycerin to deaden the nerve
- Injections of pain relievers or steroids to decrease inflammation/irritation of the nerve
- High-frequency radio waves to deaden the nerve
- Botulinum toxin injection (Botox)
Trigeminal neuralgia – Prevention
There are no guidelines for preventing TN. However, once you have it, steps that may help prevent attacks include:
- Eating soft foods
- Eating food and drinking beverages that are room temperature
- Washing your face with cotton pads and warm water
- If tooth brushing triggers attacks, rinsing your mouth with warm water after eating
- Avoiding or minimizing known triggers (eg, heat, cold, touch)