(RA; Arthritis, Rheumatoid)
Rheumatoid Arthritis – Definition
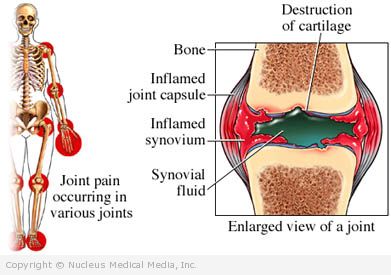
Rheumatoid arthritis (RA) is an autoimmune disease. It causes pain, swelling, stiffness, and loss of function in the joints. RA usually affects the same joint on both sides of the body. It occurs mostly in the:
- Fingers
- Wrists
- Elbows
- Shoulders
- Jaw
- Hips
- Knees
- Toes
Rheumatoid Arthritis – Causes
RA is caused by a combination of genetic and environmental factors that trigger an abnormal immune response. Possible causes:
- Genetic factors — Certain genes that play a role in the immune system are associated with RA development.
- Defects in the immune system can cause ongoing inflammation.
- Environmental factors — Certain infectious agents, such as some viruses or bacteria, may increase susceptibility to RA.
- Other factors — Some evidence suggests that hormonal factors may promote RA development in combination with genetic factors and environmental exposure.
Rheumatoid Arthritis – Risk Factors
These factors increase your chance of developing RA. Tell your doctor if you have any of these risk factors:
- Family members with RA
- Sex: female
- Ethnic background: Pima Indians
- Heavy or long-term smoking
Rheumatoid Arthritis – Symptoms
When RA begins, symptoms may include:
- Joint pain and stiffness that is:
- Symmetrical
- Most prominent in the morning
- Lasts for at least half an hour
- Red, warm, or swollen joints
- Joint deformity
- Mild fever, tiredness
- Loss of appetite
- Small lumps or nodules under the skin
As RA progresses, it may cause complications with the:
- Heart
- Lungs
- Eyes
- Skin
- Liver
- Kidneys
- Blood
- Nervous system
- Blood vessels
It is also linked to early cardiovascular disease and death.
Rheumatoid Arthritis – Diagnosis
The doctor will ask about your symptoms and medical history. You will also be examined. To be diagnosed with RA, you must have at least one swollen or tender joint or a history of a swollen joint. How many joints, and which joints are involved will help aid your doctor in coming to the diagnosis. The doctor will also rule out other conditions that may have similar symptoms, like lupus or gout.
To aid in the diagnosis, your doctor will order tests, such as:
- Blood tests to determine if you have an automimmune disease:
- Rheumatoid factor (RF)
- Anti-citrullinated protein antibody
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
- Imaging tests, such as x-rays
Rheumatoid Arthritis – Treatment
There is no cure for RA. The goals of treatment are to:
- Relieve pain
- Reduce inflammation
- Slow down joint damage
- Improve functional ability
Medications
There are a variety of medicines to treat the pain and inflammation of RA. In some cases, medicines may be used in combination.
- Disease-modifying anti-rheumatic drugs (DMARDS)—to slow the course of the disease; used early in the course of the disease to prevent long-term damage:
- Methotrexate (eg, Rheumatrex)
- Hydroxychloroquine (eg, Plaquenil)
- Sulfasalazine (eg, Azulfidine)
- Leflunomide (eg, Arava)
- Cyclosporine (eg, Neoral)
- Penicillamine (eg, Cuprimine)
- Gold (eg, Ridaura)
- Minocycline (eg, Minocin)
- Immunosuppressive drugs (only used when other DMARDS are ineffective):
- Azathioprine (eg, Imuran)
- Cyclophosphamide (eg, Cytoxan) — rarely used
- Chlorambucil (eg, Leukeran) — rarely used
- Over-the-counter medicines:
- Acetaminophen (eg, Tylenol)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) including ibuprofen and naproxen
- Biologic response modifiers — drugs that interfere with the autoimmune response; includes TNF-inhibitors, such as:
- Etanercept (eg, Enbrel)
- Infliximab (eg, Remicade)
- Adalimumab (eg, Humira)
- Golimumab (eg, Simponi)
- Certolizumab (eg, Cimzia)
Steroids
Low-dose corticosteroids (eg, prednisone) are often used first. They may be tapered when other drugs start working. Avoid long-term steroid use. Corticosteroid injections to inflamed joints may also be used.
Rest and Exercise
Rest reduces active joint inflammation and pain and fights fatigue. Exercise is important for maintaining muscle strength and flexibility. It also preserves joint mobility.
Joint Care
Splints applied to painful joints may reduce pain and swelling. Devices that help with daily activities can also reduce stress on joints. Devices include:
- Zipper extenders
- Long-handled shoehorns
- Specially designed kitchen tools
Stress Reduction
Stress reduction can ease the difficulties of living with a chronic, painful disease. Participating in an exercise program or joining a support group are two strategies you can use to reduce stress. Cognitive behavioral therapy, a form of talk therapy, and meditation may also offer benefits in reducing your pain and improving your ability to cope with RA.
Surgery
Joint replacement and tendon reconstruction help relieve severe joint damage.
Lifestyle Measures
These may relieve stiffness and weakness and reduce inflammation:
- Maintain a balance between rest and exercise.
- Attempt mild strength training.
- Participate in aerobic exercise (eg, walking, swimming, dancing).
- Avoid heavy impact exercise.
- If you smoke, quit.
- Control weight.
- Participate in a physical therapy program.
Rheumatoid Arthritis – Prevention
There are no guidelines for preventing RA.