Pulmonary embolism
Pulmonary embolism – Definition
A pulmonary embolism is a blockage of an artery in the lungs. The embolism prevents blood and nourishment from getting to a specific area of the lungs. This may lead to the death of lung tissue in this area. Damage to the lungs may make it difficult for the lungs to work properly. In severe cases, a pulmonary embolism can lead to death.
Pulmonary embolism – Causes
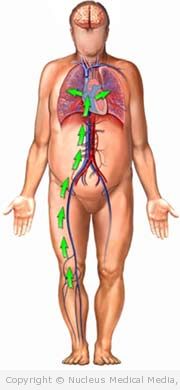
An embolism is caused by a lump of material, called an embolus, that is floating in the blood. An embolus, can be a blood clot, air bubble, or a piece of fat, bone marrow, or tumor tissue. The embolus travels from its original location and passes through larger blood vessels until it gets stuck in a smaller blood vessel. In this case, the embolus is trapped in an artery of the lungs.
The embolus in a pulmonary embolism is usually a blood clot. It most often starts in a vein in the legs or pelvis.
Pulmonary embolism – Risk Factors
Factors that increase your chance of developing pulmonary embolism include:
- Blood clot in a deep vein of a leg or pelvis
- Increased levels of clotting factors in the blood
- Prolonged bed rest
- Major surgery, especially after pelvic surgery, knee replacement, or heart surgery
- Injury to a vein in a leg or pelvis
- Fractures of the hip or thigh bone (femur)
- Certain blood disorders
- Prolonged sitting, such as during a long trip
- Pregnancy or postpartum period
- Smoking
- Obesity
- Inflammatory bowel disease
- Autoimmune disorder (eg, immune thrombocytopenic purpura, polyarteritis nodosa, polymyositis)
- Cancer
- Taking certain medicines, such as birth control pills or antipsychotics
Pulmonary embolism – Symptoms
The symptoms of pulmonary embolism vary depending on the size and location of the blockage. The area affected by the lack of blood will also affect the symptoms. In general symptoms may include:
- Shortness of breath that starts suddenly for no obvious reason
- Chest pain, especially when breathing or coughing (it can mimic a heart attack)
- Feeling faint, lightheaded, dizzy
- Cough, sometimes with bloody phlegm
- Rapid heartbeat
- Rapid breathing
- Anxiety
- Feeling of impending doom
Pulmonary embolism – Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done. Your doctor may order the following tests:
- Arterial blood gas study — a blood test to check oxygen levels and lung function
- Chest x-ray — picture of lungs to look for signs of dead tissue; a pulmonary embolism cannot be seen on the chest x-ray
- Lung perfusion scan — a test that measures breathing and circulation in all areas of the lungs. An embolus will cause a mismatch in the lungs.
- CT scan of the chest — detailed pictures of the inside of the chest.
- Pulmonary angiogram — a special dye can highlight the areas of blockage in the lungs.
- MR angiography (MRA)
- Electrocardiogram (ECG, EKG) — a test to look for abnormal rhythms in the heart like rapid heart beats, may help in diagnosis
- Echocardiography — a test to examine the size, shape, and motion of the heart
- D-Dimer (a clot dissolving substance) blood test — Increased levels in the blood may suggest the presence of a clot
- If you have a family history of blood clots and had blood clots in the past for no apparent reason, your doctor may order additional blood tests. The tests will look for possible inherited defects in your clotting system such as:
- Factor V Leiden mutation (seen in up to 40% of cases)
- Increased factor VIII
- Additional tests may be done to check blood flow or look for clots in the veins. Most likely done in legs.
If you are diagnosed with pulmonary embolism, follow your doctor’s instructions.
Pulmonary embolism – Treatment
Treatment depends on the size and severity of the clot. Emergency treatment and hospitalization may be needed.
Treatments include:
Medicine
The first step in treatment is a blood thinner (anticoagulant medication).
- Enoxaparin (Lovenox)
- Fondaparinux (Arixtra)
- Heparin
After the initial period, the blood thinner medication will be switched to a longer acting anticoagulant. One example is warfarin.
Another type of medication may be needed to dissolve the clot. These are called thrombolytic medicines and include alteplase (Activase) and urokinase (Kinlytic). This type of medication is usually only used in patients with a very large PE or a PE that is causing severe illness. Thrombolytics will not be used if you have a high risk of bleeding.
Surgery
A surgery to remove the clot may be needed if the blockage is very large. The surgery is called an embolectomy.
Clot-Trapping Filter
Some may have repeated problems with blood clots. In this case, a surgery will be done to place a filter in the main vein of the legs. This filter will trap clots before they can travel to the lungs.
Pulmonary embolism – Prevention
Prevention of pulmonary embolism means preventing clots from forming.
You can help prevent clots with a healthful lifestyle:
- Eat a healthful diet, one that is low in saturated fat and rich in whole grains, fruits, and vegetables.
- Begin a safe exercise program with the advice of your doctor.
- Walk or move your legs to break up long periods of sitting.
- If you smoke, quit.
- Unless you are on a fluid-restricted diet, be sure to drink lots of water.
People at high risk of developing blood clots can do the following:
- Take medicine, if your doctor recommends it. Anticoagulant drugs are most commonly used.
- Wear elastic stockings (also called support hose) if suggested by your doctor. They can help to improve circulation in your legs.
- Walk or move your legs to break up long periods of sitting. If your are traveling, get up and walk every few hours.