Heart failure
(Congestive Heart Failure; Chronic Heart Failure; Left Ventricular Dysfunction; Left Ventricular Failure)
Heart failure – Definition
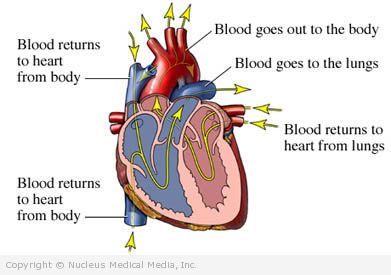
In heart failure, the heart is unable to pump the right amount of blood throughout the body. This causes blood to back up in the veins. Depending on which part of the heart is affected most, this can lead to a build up of excess fluid in the lungs, feet, and elsewhere. Heart failure can worsen with time, which may lead to the use of many treatments. Because of this, doctors are aggressive in treating heart failure to try to prevent it from worsening.
Heart failure – Causes
The leading causes of heart failure are:
- Coronary artery disease
- Heart attack
Other common causes include:
- Problems with the heart’s valves due to:
- Rheumatic heart disease
- Bacterial endocarditis
- Congenital defects
- Calcium deposits from atherosclerosis
- High blood pressure
- Diabetes
Other less common causes include:
- Cardiomyopathy (weakened, damaged heart muscle from various causes)
- Certain medicines
- Abnormal heartbeats ( arrhythmias)
- Hyperthyroidism (overactive thyroid)
- Amyloidosis
- Kidney failure and/or liver failure
- Thiamine ( vitamin B1) deficiency
Heart failure – Symptoms
Symptoms include:
- Shortness of breath — at first only with activity, then progressing to shortness of breath at rest
- Unexplained weight gain
- Swelling of feet, ankles, or legs
- Need to sleep propped up
- Fatigue, weakness
- Wheezing
- Cough — may be dry and hacking or wet sounding, may have a pink, frothy sputum
- Frequent urination, especially at night
- Abdominal pain
Heart failure – Risk Factors
Risk factors include:
- Advancing age
- Obesity
- Excess intake of salt and fat
- Excess alcohol intake
- Sex: male
- Race: Black
- Smoking
- Pregnancy
- High fever
- Severe infection
- Chronic lung disease ( emphysema)
- Chemotherapy
Heart failure – Diagnosis
The doctor will ask about your symptoms and medical history. She will also do a physical exam, which will include:
- Listening to your lungs and heart with a stethoscope
- Examining the veins in the neck
- Feeling the abdomen for tenderness and liver swelling
- Checking your feet, ankles, and legs for swelling
Tests may include:
- Blood tests — to look for certain markers in the blood that help the doctor determine what is happening with your heart
- Urine tests — to look for certain markers in the urine that help the doctor determine what is happening with your heart
- Electrocardiogram (ECG, EKG) — records the heart’s activity by measuring electrical currents through the heart muscle
- Echocardiogram — uses high-frequency sound waves (ultrasound) to examine the size, shape, function, and motion of the heart
- Exercise stress test — records the heart’s electrical activity during increased physical activity (may be coupled with echocardiogram or nuclear scan)
- If you cannot exercise, you may be given medicine. This medicine simulates physical exertion.
- Nuclear scanning — uses radioactive material (such as thallium) to highlight areas with diminished flow
- Coronary angiography — uses a catheter, dye, and x-rays to look for abnormalities (eg, narrowing, blockage) in the arteries and evaluate the function of the heart
Heart failure – Treatment
Treatment of Underlying Conditions
Heart failure may be caused by another condition. Treating this condition should improve your heart failure or prevent if from getting worse.
Lifestyle Changes
The following lifestyle changes can help treat the symptoms of heart failure and slow down its progression:
- Avoid alcohol.
- If you smoke, quit.
- Lose weight if needed.
- Eat a healthy diet. Your diet should be low in fat and salt and high in fiber.
- Ask your doctor if you need to restrict fluids. Find out how much salt and fluid is right for you.
- Begin an exercise program with guidance from your doctor. Aerobic training may help improve your level of physical activity and quality of life. You should aim to exercise for 20-30 minutes at least five times each week. You can begin slowly and work your way to this goal. Talk to your doctor before you start an exercise program.
- Weigh yourself every morning. This will allow you to quickly detect if you are retaining fluid. Call your doctor if you gain three or more pounds in one day, five or more pounds in one week, or whatever amount you were told to report. The best time to weigh yourself is before breakfast and after urinating. You should weigh yourself while wearing the same type of clothes, without shoes, and on the same scale. This will help you to know that your weight is accurate.
Medicines
Your doctor will most likely prescribe a combination of medicines, such as:
- ACE inhibitors or their alternatives to widen blood vessels
- Digoxin (also called digitalis) to help your heart pump
- Beta-blockers to slow your heart rate and lower blood pressure
- Diuretics to remove excess fluid in your body
- Nitrates to dilate the blood vessels
You may also be given medications to:
- Thin the blood (eg, aspirin, warfarin [eg, Coumadin])
- Help manage chest pain (eg, nitroglycerin)
- Help manage cholesterol levels
- Help control high blood pressure
If heart failure worsens, you may need medical devices to help your heart pump blood properly. If you have heart failure, follow your doctor’s instructions.
Heart failure – Prevention
The best way to prevent heart failure is to reduce your risk of:
- Coronary artery disease
- High blood pressure
- Diabetes
Take these steps to reduce your risk:
- Begin a safe exercise program with the advice of your doctor.
- If you smoke, quit.
- Limit alcohol.
- Lose weight if needed. Once you have lost weight, maintain a healthy weight.
- Eat a healthy diet. The DASH diet, in particular, may reduce the risk of high blood pressure and heart failure, particularly in women. The DASH diet is:
- Rich in fruits, vegetables, and low-fat dairy foods
- Low in saturated fat, total fat, and cholesterol
- Eat whole grain breakfast cereal. In addition to the other healthy habits, this may reduce your risk.