Peripheral Neuropathy
Peripheral neuropathy – Definition
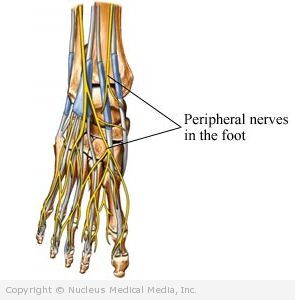
Peripheral neuropathy is damage to the peripheral nerves. These are the nerves that connect your spinal cord to the rest of your body.
Peripheral neuropathy – Causes
Many diseases and conditions can cause peripheral neuropathy. The damage may occur due to:
- Malnutrition
- Compression (from repetitive stress)
- Cancer
- Trauma
- Inflammation of nerves or blood vessels
- Infection
- Toxins
- Medications
- Hereditary syndromes
- Unknown causes
Diseases that can damage peripheral nerves include (but are not limited to):
- Diabetes ( type 1 or type 2)
- Alcoholism
- AIDS
- Lyme disease
- Rheumatoid arthritis
- Uremia from chronic kidney failure
- Autoimmune disorders
- Hypothyroidism
- Viral infections (such as hepatitis)
Compression commonly occurs when nerves are pinched or trapped somewhere along their course, such as:
- Carpal tunnel syndrome (nerve in the wrist)
- Sciatica (nerve roots forming the sciatic nerve in the back of the legs as they exit the spine)
Toxins that can damage the peripheral nerves include:
- Lead
- Mercury
- Thallium
- Organic solvents (hexacarbons)
- Pesticides (organophosphates)
- Carbon disulfide
- Arsenic
- Acrylamide
- Diphtheria toxin
- Alcohol
Many medicines can lead to peripheral neuropathy. A partial list includes:
- Chemotherapeutic agents to treat cancer (eg, vincristine, paclitaxel, cisplatin)
- Anti-HIV medications (eg, didanosine, zalcitabine)
- Anti- tuberculosis medications (eg, isoniazid, ethambutol)
- Other antimicrobial drugs (eg, dapsone, metronidazole, chloroquine, chloramphenicol)
- Psychiatric medications (eg, lithium)
- Other medications (eg, amiodarone, aurothioglucose, phenytoin, thalidomide, colchicine, cimetidine, disulfiram, hydralazine, high levels of vitamin B6)
Other causes of peripheral nerve damage include:
- Vitamin deficiencies ( thiamin and B12 deficiency, vitamin E deficiency)
- Injury
- A tumor pressing on a nerve
- Exposure to cold or radiation
- Leprosy
- Acute or chronic demyelinating polyneuropathy
- Porphyria
- Paraneoplatic syndromes
- Genetic disorders ( Charcot-Marie-Tooth disease or hereditary motor and sensory neuropathy)
- Prolonged treatment in the intensive care unit
Peripheral neuropathy – Risk Factors
These factors increase your chance of developing this condition. Tell your doctor if you have any of these risk factors:
- Diabetes (about 60% of people with diabetes have peripheral neuropathy)
- Alcohol abuse
- Autoimmune diseases, such as rheumatoid arthritis or celiac sprue
- Family member with peripheral neuropathy
- Exposure to toxins or medications known to cause neuropathy
- Vitamin deficiency (thiamin and vitamin B12)
- HIV infection
- Pressure on a nerve (may occur with repetitive stress injuries)
- Hospitalization treatment in the intensive care unit
Peripheral neuropathy – Symptoms
Damage to the peripheral nerves often results in sensory (feeling) and motor (strength) symptoms in the:
- Arms
- Legs
- Hands
- Feet
Other parts of the body can also be affected. Symptoms depend on which nerves are involved. They can range from mild to severe and may seem worse at night. Sensations and pain may occur in the upper or lower limbs and move toward the trunk (eg, from the feet to the calves).
Symptoms include:
- Numbness or reduced sensation
- Tingling
- Pain, often a burning or sharp, cutting sensation
- Sensitivity to touch
- Muscle twitches
- Muscle weakness
- Muscle cramping
- Difficulty with walking
- Loss of coordination or balance
- Paralysis
If untreated, peripheral neuropathy can lead to:
- Loss of reflexes and muscle control
- Muscle atrophy (loss of muscle bulk)
- Foot deformities
- Foot ulcers
- Injuries to the feet that go unnoticed and become infected
- Autonomic dysfunction (sweating, bowel and bladder dysfunction, cardiovascular effects)
- Difficulty breathing
Peripheral neuropathy – Diagnosis
The doctor will ask about your symptoms and medical history. She will also do a physical exam, which may include:
- Muscle strength
- Reflexes
- Balance
- Coordination
- Ability to feel vibration, temperature, and light touch
- Semmes-Weinstein monofilaments test — measures sensation in the feet using a fine flexible wire
Additional tests may also include:
- Blood tests (including glucose, vitamin B12 level, and thyroid function tests)
- Electromyography (EMG) — measures and records electrical activity generated in muscle in response to nerve stimulation
- Nerve conduction studies (NCS) — measures the speed and degree of electrical activity in a nerve to determine if it is functioning normally
- Serum/urine electrophoresis (protein analysis)
- Genetic testing
- Evaluation of family members
- Spinal tap (lumbar puncture, LP)
- Nerve or muscle biopsy (rarely)
- Imaging tests (eg, MRI scan, CT scan)
Peripheral neuropathy – Treatment
Treatment may include:
Treatment for the Underlying Illness or Exposure
Treating the underlying illness can decrease or eliminate symptoms. For instance, if it is caused by diabetes, controlling blood sugar levels may help. In some cases, neuropathy caused by medications or toxins is completely reversed when these substances are stopped or avoided. Correction of vitamin B12 deficiency often improves symptoms.
Physical Therapy
Certain exercises may help stretch shortened or contracted muscles and increase joint flexibility. In long-standing cases, splinting the joint may be required to protect and rest it, while maintaining proper alignment.
Orthotics (supports and braces) may help with:
- Deformities
- Balance issues
- Muscle weakness
Maintaining physical activity is also key.
Medications
Prescription and over-the-counter (OTC) pain medicines are often used to ease discomfort.
Drugs to treat depression and prevent convulsions sometimes relieve neuropathy symptoms. These medicines are often given at lower dosages. Commonly used antidepressants include:
- Amitriptyline (Elavil)
- Nortriptyline (Pamelor)
- Desipramine (Norpramin)
- Imipramine (Tofranil)
- Duloxetine (Cymbalta)
Commonly used anticonvulsants may include:
- Gabapentin (Neurontin)
- Carbamazepine (Tegretol)
- According to the Food and Drug Administration (FDA), patients of Asian ancestry who have a certain gene, called HLA-B*1502, and take carbamazepine are at risk for dangerous or even fatal skin reactions. If you are of Asian descent, the FDA recommends that you get tested for this gene before taking carbamazepine. If you have been taking this medication for a few months with no skin reactions, then you are at low risk of developing these reactions. Talk to your doctor before stopping this medication.
- Pregabalin (Lyrica) — recently approved for peripheral neuropathy
For severe and potentially life-threatening cases (such as Guillain-Barre syndrome), treatment includes:
- Intravenous immunoglobulins
- Plasmapheresis (done to exchange plasma in the blood)
Other Therapies
These therapies are aimed at reducing symptoms and may include:
- Relaxation training
- Biofeedback
- Walking
- Exercise
- Yoga
- Warm baths
- Massage
- Acupuncture
- Transcutaneous electronic nerve stimulation
Surgery
Surgery can relieve the pressure on nerves. For example, surgeons commonly release fibrous bands in the wrist to treat carpal tunnel syndrome.
Peripheral neuropathy – Prevention
- Manage chronic medical conditions with the help of your doctor. If you have diabetes, visit a podiatrist for yearly exams.
- Eat a healthful diet, one that is low in saturated fat and rich in whole grains, fruits, and vegetables.
- Be sure to get the right amounts of thiamin and vitamin B12.
- Limit your alcohol intake to a moderate level. This means two or fewer drinks per day for men and one or fewer for women.
- Avoid:
- Toxic chemicals
- Repetitive movements
- Prolonged pressure on joints, especially elbows and knees