Familial adenomatous polyposis
Familial adenomatous polyposis – Definition
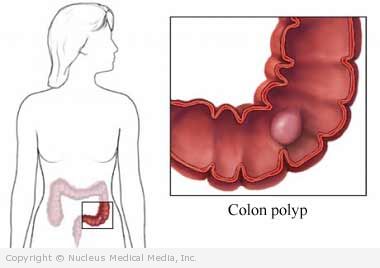
Familial adenomatous polyposis (FAP) is a rare, inherited type of colorectal cancer. FAP results in the development of hundreds of polyps inside the large intestine.
Familial adenomatous polyposis – Causes
FAP is caused by a genetic defect. Polyps usually begin developing during puberty, and 90% of people with FAP will have polyps by age 25. By the age of 40, one or more of these polyps will become cancerous.
Familial adenomatous polyposis – Risk Factors
A risk factor is something that increases your chances of getting a disease or condition. The primary risk factor for FAP is having family members with this condition.
Familial adenomatous polyposis – Symptoms
In the early stages, there may be no symptoms. When symptoms do occur, they may include:
- Bright red blood in the stool
- Diarrhea
- Constipation
- Cramping pain in the stomach
- Consistent decrease in the size of stool
- Weight loss
- Bloating
- Fatigue
Familial adenomatous polyposis – Diagnosis
Your doctor will ask about your symptoms and medical history and perform a physical exam. Tests may include:
- DNA analysis — Blood samples are taken from members of your family to determine if you have the defective gene.
- Endoscopy — A thin, lighted, telescope-like tube is inserted into the colon to check for polyps. This may be:
- A limited exam of the rectum with a proctoscope
- A more extensive exam of the rectum and sigmoid colon with a sigmoidoscope
- A complete exam of the entire large intestine with a colonoscope
- Biopsy — If a polyp is found during endoscopy, a small sample will be removed and sent to a lab for testing.
Familial adenomatous polyposis – Treatment
FAP is treated with surgery. Since FAP causes so many polyps, they cannot be removed individually. Therefore, the goal of surgery is to remove the portion of the intestine that contains the cancerous or precancerous polyps. The surgical procedure used depends on the length of intestine involved.
For reasons not entirely understood, rectal polyps will often regress or disappear after a more limited surgery that does not require the removal of the rectum. Therefore, often times the surgeon will leave the rectum in place and remove the rest of the large bowel. If the polyps in the rectum do not disappear, then the rectum will likely need to be removed as well.
The three main surgical treatments are:
Colectomy With Ileorectal Anastomosis (IRA)
This is the most common procedure for patients with few polyps in the rectum. The colon is removed, but five inches of the rectum remain. The small intestine is surgically joined to the upper rectum. This procedure preserves sphincter tone and allows for relatively normal sensation of the need to have a bowel movement.
Restorative Proctocolectomy (Pouch)
The colon and rectum are removed, leaving the anal canal and anal sphincter muscles. An artificial rectum (pouch) is created from the lower end of the small intestine. The pouch is attached to the anus, so bowel actions can be controlled. This operation is usually done in two stages.
Total Proctocolectomy With Permanent Ileostomy
The colon, rectum, and anus are removed. Then, a permanent ileostomy (opening in the abdomen) is created. A bag is attached to collect waste through the ileostomy. This type of surgery is not used very often anymore, unless the rectum contains many polyps and they do not regress after a lesser surgery.
Follow-Up
If only a portion of the bowel is removed at surgery, the remaining bowel will need to be inspected by endoscopy every 3-6 months for the rest of your life. Because the risk of developing other polyps that could grow to become cancer is so high, it is crucial for your doctor to keep a very close watch on the remaining bowel. If more polyps arise, further surgery may be required.
Familial adenomatous polyposis – Prevention
There are no guidelines for the prevention of FAP.
There are some preliminary studies evaluating the use of cyclooxygenase antagonists (Vioxx or Celebrex) to prevent the development of colorectal polyps. However, it is too early to tell if these drugs have any effect on the development of cancerous polyps in FAP.