Barrett’s esophagus
Barrett’s esophagus – Definition
Barrett’s esophagus is a complication of chronic esophagitis, which is inflammation of the esophagus.
Barrett’s esophagus is characterized by a change in the cells lining the esophagus. Normal cells are flat-shaped (squamous) cells, while Barrett’s esophagus cells are shaped like a column. This cell change is called metaplasia. It is a premalignant phase that may eventually result in cancer of the esophagus if untreated.
Barrett’s esophagus – Causes
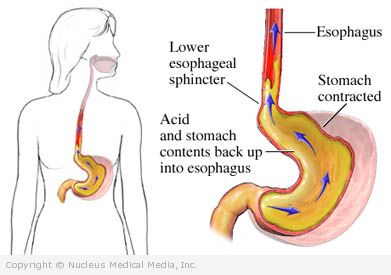
The exact cause of Barrett’s esophagus is unknown. However, it may result from damage to the esophagus caused by the chronic reflux of stomach acid. Frequent or chronic reflux of stomach acid into the esophagus is called gastroesophageal reflux disease, or GERD.
Barrett’s esophagus – Risk Factors
A risk factor is something that increases your chance of getting a disease or condition. Risk factors include:
- Chronic heartburn
- History of GERD
- Age: 50 and over
- Sex: male
- Hiatal hernia
- Unhealthy eating habits
Barrett’s esophagus – Symptoms
Although Barrett’s esophagus does not directly produce symptoms, people with GERD may experience the following:
- Heartburn
- Chest pain
- Nausea or vomiting
- Blood in vomit or stool
- Sore throat or chronic cough
- Hoarse voice
- Sour taste in mouth (acid reflux)
- Shortness of breath or wheezing
- Difficulty or pain with swallowing ( dysphagia)
Barrett’s esophagus – Diagnosis
The doctor will ask about your symptoms and medical history, and perform a physical exam. Tests may include:
- Biopsy — removal of a sample of tissue from the esophagus during the endoscopy to be tested for cancer cells
- Endoscopy — a thin, lighted tube inserted down the throat to examine the esophagus
Barrett’s esophagus – Treatment
Once the cell changes of Barrett’s esophagus occur, the changes are permanent. The goal of treatment is to prevent further damage by stopping the reflux of acid from the stomach. Treatment may include:
Medications
The following types of medicines may be prescribed:
- H2-blockers, such as:
- Cimetidine (Tagamet)
- Ranitidine (Zantac)
- Famotidine (Pepcid)
- Nizatidine (Axid)
- Proton pump inhibitors, such as:
- Omeprazole
- Lansoprazole
- Pantoprazole (Protonix)
- Rabeprazole (Aciphex)
Surgery
If the disease is severe or the medicine is unsuccessful, your doctor may recommend surgery. Surgical options may include:
- Fundoplication —part of the upper stomach is wrapped around the esophagus; this is done to reduce further damage caused by GERD
- Esophagectomy—removal of the Barrett’s segment of the esophagus
- Ablation of the abnormal lining by several methods — photodynamic therapy (PDT), argon plasma coagulation (APC), multipolar electrocoagulation (MPEC), heater probes, lasers, cryotherapy, and radiofrequency ablation (Most of these techniques are investigational, except for PDT.)
Monitoring
Your doctor may recommend endoscopy about (or at least) every 1-3 years to monitor the esophagus for early signs of cancer. This recommendation must be individualized for each person.
Barrett’s esophagus – Prevention
The best way to prevent Barrett’s esophagus is to minimize and/or treat the reflux of stomach acid into the esophagus, which is usually due to GERD. In addition to drugs or surgery, self-care measures for GERD include:
- Do not smoke. If you smoke, quit.
- If you are overweight, lose weight.
- Elevate the head of your bed on 4-6 inch blocks.
- Avoid clothes with tight belts or waistbands.
- Avoid foods that cause heartburn. These include alcohol, caffeinated beverages, chocolate, and foods that are fatty, spicy, or acidic (such as citrus or tomatoes).
- Eat 4-6 small meals per day.
- Do not eat or drink for 3-4 hours before you lie down or go to bed.