(Pressure Ulcers; Bed Sores; Decubitus Ulcers)
Pressure Sores – Definition
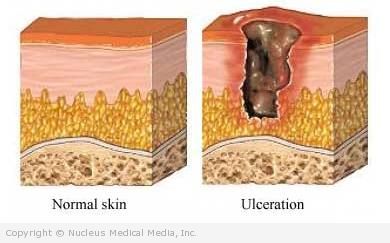
A pressure sore is a lesion that develops on the skin and underlying tissues due to unrelieved pressure usually over a bony prominence. The skin and tissues rely on an adequate blood supply for oxygen and nutrients. When tissues are compressed for an extended period from hours to days, blood supply can be cut off, leading to development of a sore.
Pressure Sores – Causes
Pressure sores result from lying or sitting in one position for too long a time. Prolonged pressure cuts off the blood supply to tissues that are compressed between a bony area and a mattress, chair, or other object. Without oxygen and nutrients, the tissue starts to die.
Several factors contribute to the development of pressure sores including:
- Pressure — Pressure sores can result from the inability to change position or to feel discomfort caused by pressure. People with normal mobility and sensation change position automatically, without thinking.
- Friction — Even friction from pulling someone across bed sheets can damage small blood vessels that supply the skin tissue.
- Poor nutrition
- Moisture — This can come from sweating due to an elevated temperature (fever) or leakage of urine or stool.
- Obesity — Extra weight increases pressure on the skin over the bones and joints.
Pressure Sores – Risk Factors
A risk factor is something that increases your chance of getting a disease or condition.
- Immobility, such as being bed- or chair-bound
- Sensory loss
- Poor nutrition
- Incontinence, or leakage of urine or stool
- Advanced age
- Chronic or complex medical problems, such as:
- Anemia
- Infection
- Poor circulation
- Neuropathy
- Dementia
- Cancer
- Diabetes
- Stroke
- Spinal cord injury or paralysis
- Bone fracture
- Swelling or water retention
- Dry skin
- Fever
Pressure Sores – Symptoms
Symptoms of a pressure ulcer may include:
- Skin tissue that feels firm or boggy
- Local redness, warmth, tenderness, or swelling
- Reddish or purplish skin discoloration, often over a bony area
- Pain or itching of the skin
- Blistering, sores, skin breakdown, or drainage
If the redness remains a half hour after the pressure has been removed, the skin will likely break down. The reddened area may blister and a shallow ulcer may develop. Fluid may drain. The wound can deepen and can extend through fat and muscle to the bone. The area may be painful. The wound can become infected, with redness, swelling, odor, pus, warmth, and fever. If untreated, the infection can progress to gangrene, a blood infection, or an infection of the bone beneath.
Pressure Sores – Diagnosis
The doctor will ask about your symptoms and medical history, and perform a physical exam. The doctor will examine the ulcer and note the location, shape, size, depth, stage, and any formation of pockets or cavities. Pressure sores are staged according to the depth and tissues that are involved.
Tests may include:
- Wound culture — taking a sample of material from a sore to be tested for bacteria
- Blood tests — to check for infection and nutritional status
- X-ray or bone scan — if bone infection is suspected
Pressure Sores – Treatment
Treatment aims to relieve pressure on the area, heal the wound, avoid complications, and prevent future pressure sores. In many cases, a caregiver will provide care for your pressure sores.
Treatment includes:
Positioning
- Avoid placing any weight or pressure on the wound.
- Change position at least every two hours, around the clock.
- Maintain good body alignment.
- Make sure bedclothes are clean and without wrinkles.
- If needed, use a special mattress.
- Use a “lift sheet” to move the patient rather than pulling the bedsheet or the patient.
Hygiene
Clean soiled skin after each bowel movement and urination. Wash with mild soap and warm water. Rinse well. Pat dry. Do not rub. Apply lotion as recommended by the doctor.
Wound Care
A nurse or doctor will teach you or your caregiver how to tend to the wound. Some basic instructions include:
- Clean the sore, remove dead tissue, and apply a dressing.
- Do not put anything else on the ulcer.
- Wash hands before and after performing wound care.
- Clean the wound every time the bandage is changed.
- You may need to take pain medication a half hour or hour before dressing changes.
Nutrition
Eat a well-balanced meal. Your doctor may recommend vitamins, minerals, or supplements.
Surgery and Other Procedures
The doctor may surgically remove dead tissue and skin grafts may be needed. In some situations, electrotherapy may be used to stimulate blood flow and promote healing.
If you are diagnosed with pressure sores, follow your doctor’s instructions.
Pressure Sores – Prevention
Most pressure ulcers can be prevented. Suggestions include:
- Follow these tips when repositioning:
- Change position in bed at least every two hours or, in a wheelchair, at least hourly. If able to move yourself, shift position every 15 minutes.
- Maintain good body alignment.
- To prevent sliding, do not elevate the head of the bed greater than 30°. Discuss the bed elevation with your doctor in case this is contraindicated because of risk of difficulty breathing, choking, or aspiration.
- Find a sitting or lying position that is 30° toward one side or the other, but not squarely on the hip.
- Place a pillow under calves to keep the heels off the mattress.
- Place a pillow between the knees.
- Do not use donut-ring cushions, which can cut off circulation.
- Talk to the doctor about using:
- A special foam mattress designed to reduce the risk of pressure sores
- A mechanical mattress or overlay (goes over the mattress) that inflates and deflates to change the pressure on the body
- Sheepskin overlay
- Use a special cushion on the wheelchair.
- Wear special pads to protect skin that is resting against braces and other devices.
- When moving someone, lift rather than drag.
- Use assistive devices, such as transfer boards and mechanical lifts.
- Try placing a sheepskin under a body part to decrease friction.
- Keep the skin clean and dry.
- Do not massage bony areas.
- If incontinent, use a protective cream on skin that may come in contact with urine or stool. Frequently check the patient, and do not let feces or urine remain for extended periods of time
- Check the skin at least daily for signs of pressure problems.
- Keep sheets clean and free of wrinkles
- Maintain good nutrition.