Hip replacement
(Hip Arthroplasty; Arthroplasty, Hip; Total Hip Replacement; Minimally Invasive Total Hip Replacement; Mini-incision Hip Replacement)
Hip replacement – Definition
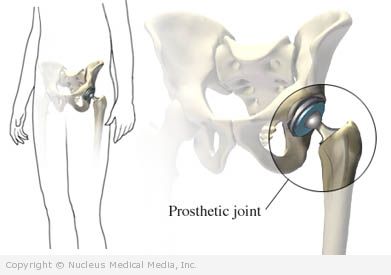
A total hip replacement is a surgery to replace a diseased or injured hip joint. An artificial ball-and-socket joint is inserted to make a new hip. The artificial joint is called a prosthesis.
A minimally invasive total hip replacement is also a surgery to replace a diseased or injured hip joint. This surgery only requires one or two tiny incisions and special instruments. People eligible for this surgery are typically:
- Younger than 50
- Normal weight
- Healthier than those who undergo the traditional total hip replacement surgery
Hip replacement – Reasons for Procedure
This surgery is done when pain and stiffness limit your normal activities. This pain and stiffness is usually due to arthritis. Surgery is done when other treatments have been tried and are no longer working. These other treatments include rest, medicines, and physical therapy.
Within six weeks, you should be able to resume normal light activities. A replacement hip typically lasts 10-15 years.
Hip replacement – Possible Complications
If you are planning to have a hip replacement, your doctor will review a list of possible complications, which may include:
- Hip dislocation (most common complication) — occurs when the ball portion of the prosthesis dislocates from its normal position in the hip
- Infection
- Blood clots
- Swelling or bleeding
- Injury to nearby nerves or blood vessels
- Anesthesia-related problems, like pneumonia
- Noisy or “squeaky” hip after surgery
Factors that may increase the risk of complications include:
- Pre-existing medical condition (eg, heart or lung problems)
- Obesity
- Infection (eg, urinary tract infection, gum disease) — Having an infection increases the risk of bacteria entering the bloodstream and infecting the joint.
- Previous problems with blood clots
- Smoking
Be sure to discuss these risks with your doctor before the surgery.
Hip replacement – What to Expect
Prior to Procedure
Your doctor may do the following:
- Physical exam
- X-rays — a test that uses radiation to take a picture of structures inside the body
- Blood tests
- MRI scan — a test that uses a magnetic field to make pictures of structures inside the body
- CT Scan — a special type of x-ray that uses a computer to make pictures of structures inside the body
In the time leading up to the procedure:
- Try to lose weight if you are overweight. This will decrease the amount of stress on your new joint. Pool exercise may be a good option.
- To enhance safety and recovery, make home modifications:
- Install safety bars, a raised toilet seat, a shower bench, and hose. Install handrails on stairways and steps.
- Remove throw rugs. Check to make sure extension cords are in a safe place.
- Purchase a stable, firm-backed arm chair. When seated, your knees should remain lower than your hips.
- Buy items to make daily activities easier (eg, reachers, dressing aids).
- Place items so that they are easy to reach. This way, you will be able to avoid bending.
- Talk to your doctor about your medicines. You may be asked to stop taking some medicines up to one week before the procedure, like:
- Anti-inflammatory drugs (eg, aspirin)
- Blood thinners, like clopidogrel (Plavix) or warfarin (Coumadin)
- Your doctor may suggest donating your own blood for the surgery. You will most likely lose some blood and fluid during this surgery. If you need a blood transfusion, the doctor can use your own blood.
- If you become sick or have a fever just before the surgery, tell your doctor right away.
- Arrange for a ride to and from the hospital. Also, arrange for help at home.
- If you smoke, try to smoke less or stop smoking.
- Eat a light meal the night before the surgery. Do not eat or drink anything after midnight. If you have diabetes, ask your doctor if you will need to adjust your medicine.
Hip replacement – Anesthesia
General anesthesia will be used. It will block any pain and keep you asleep through the surgery. It is given through an IV in your hand or arm.
Hip replacement – Description of the Procedure
Total Hip Replacement
The doctor will make an incision along your joint. The muscles will be moved aside. The damaged bone and cartilage of the hip joint will be removed. The doctor will then prepare the remaining bone for the prosthesis. The new plastic and metal joint will be placed in position. Depending on the type of prosthesis, the doctor may use bone cement to hold one or both parts of the artificial hip firmly to your bone. Lastly, the incision will be closed with stitches or staples.
Minimally Invasive Total Hip Replacement
This surgery may be done with one or two incisions.
For both types, special tools are used that fit into these small incisions. In some cases, x-rays will be used to help guide the doctor.
For the one-incision surgery, the doctor will make an incision over the outside of your hip. The doctor will move the muscles and tendons out of the way. Next, the damaged bone and cartilage of the hip joint will be removed. The doctor will prepare the remaining bone for the prosthesis. The new plastic and metal joint will then be placed in position. Depending on the type of prosthesis, bone cement may be used to hold the artificial hip in place. Lastly, the incision will be closed with staples or stitches.
In a two-incision surgery, the doctor will make an incision over the groin and another over the buttock. The above process will then be followed.
Hip replacement – How Long Will It Take?
- Total hip replacement: 1-1½ hours
- Minimally invasive total hip replacements: 1 or more hours
Hip replacement – How Much Will It Hurt?
You will have pain after the surgery. Pain medicine will be given to help with pain.
Hip replacement – Average Hospital Stay
This procedure is done in a hospital setting. The usual length of stay is:
- 4-6 days for a total hip replacement
- 1-2 days for minimally invasive total hip replacement
Your doctor may choose to keep you longer, if complications arise. In some case, you may need to stay in a rehab unit. The focus will be on regaining function.
Hip replacement – Post-procedure Care
At the Hospital
While you are recovering at the hospital, you may need to:
- Walk with help, using a walker, on the day after surgery.
- Be careful. A fall can damage or dislocate the new joint. Do not try to walk without help.
- Take medicine to prevent blood clots.
- Wear compression boots or stockings.
- Begin physical therapy to regain mobility and strength.
- Breathe deeply and cough 10-20 times every hour — This will decrease the risk of fluid build-up in the lungs. The fluid can cause pneumonia.
At Home
When you return home, do the following to help ensure a smooth recovery:
- Keep the incision area clean and dry.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- When seated, place a V-shaped pillow between your legs. This will help you to maintain correct positioning of your hip.
- Work with the physical therapist. You will learn how to move your hip and maintain proper alignment. You should also talk to your doctor and physical therapist about ways to prevent dislocations. Depending on your surgery, you may need to avoid crossing your legs, flexing your hips more than 90 degrees, and turning your feet very far inward or outward.
- Only take medicines recommended by your doctor. Do not take over-the-counter remedies without your doctor’s approval.
- Inform your dentist of your surgery. You may need antibiotics for some dental procedures. This will decrease the risk of bacteria entering the bloodstream and traveling to the prosthesis.
- Maintain a healthy weight. Obesity can increase wear on your new joint.
- Avoid jogging and other high-impact sports. This can also increase wear on the joint, cause it to loosen, and cause pain.
- Be sure to follow your doctor’s instructions.
Hip replacement – Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or discharge around incision site
- Pain and/or swelling in the feet, calves, or legs
- Cough, shortness of breath, chest pain
- Severe nausea or vomiting
- Hip pain that you cannot control with the medicines you have been given or that becomes worse
- Numbness, tingling, or loss of feeling in your leg, knee, or foot
- Pain, burning, urgency or frequency of urination, or persistent bleeding in the urine
In case of an emergency, call for medical help right away.