Deep vein thrombosis
(DVT; Thrombophlebitis)
Deep vein thrombosis – Definition
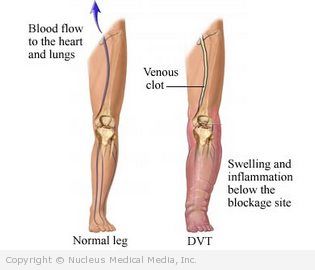
Deep vein thrombosis (DVT) is a blood clot in a vein deep in the body. Veins are blood vessels with valves that help prevent backward blood flow. Blood is pushed through the veins in legs and arms when muscles contract.
Deposits of red blood cells and clotting elements in the blood can build up in a vein. This build up leads to a blood clot. Clots usually occur in the legs but can occur in other locations. As the clot grows, it blocks blood flow in the vein.
Deep vein thrombosis – Causes
Several factors contribute to clot formation, including:
- Slow blood flow, often due to lying or sitting still for an extended period of time
- Pooling of blood in a vein, often due to:
- Immobility
- Medical conditions
- Damage to valves in a vein or pressure on the valves, such as during pregnancy
- Injury to a blood vessel
- Clotting problems (can occur due to aging or disease)
- Catheters placed in a vein
Deep vein thrombosis – Risk Factors
Risk factors for DVT include:
- Personal or family history of deep vein thrombosis
- Hospitalization
- Not moving your body
- Surgery, especially involving bones or joints
- Medical conditions, such as:
- Varicose veins
- Cancer
- Heart failure
- Heart attack
- Inflammatory bowel disease
- Blood disorders
- Blood poisoning (sepsis)
- Obesity
- Pregnancy
- Genetic factors whether inherited or by natural changes in life can change your body protein levels
- Take certain medications such as birth control pills, estrogen therapy, or antipsychotic medicine
Deep vein thrombosis – Symptoms
Symptoms occur when:
- The clot interferes with blood flow in the vein.
- Local inflammation occurs.
- A clot breaks free and travels to the lungs.
Some patients may not have any symptoms until the clot moves to the lungs. This condition is called pulmonary embolism.
Symptoms of DVT may include:
- Pain
- Swelling of a limb
- Tenderness along the vein, especially near the thigh
- Warmth
- Redness, paleness, or blueness of the skin of the affected limb
Deep vein thrombosis – Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done.
Tests may include:
- Blood tests to look for blood clotting proteins
- Duplex venous ultrasound — uses sound waves to detect changes in blood flow
- Venography — x-rays taken after dye is injected into a small vein to show areas of normal and abnormal blood flow
- Impedance plethysmography — measures changes in blood volume in the veins as a blood pressure cuff wrapped around the thigh is inflated and deflated
Deep vein thrombosis – Treatment
Treatment aims to:
- Prevent pulmonary embolism
- Stop the clot from growing
- Dissolve the clot (sometimes)
Treatments include:
Supportive Care
This may include:
- Resting in bed
- Elevating the affected limb above the heart
- Wearing compression stockings as recommended by your doctor
Medications
Anticoagulant drugs to prevent additional clot formation include:
- Heparin injection — fast-acting drug that prevents more clot formation; given for several days
- Can be of normal or low-molecular weight ( Lovenox)
- Warfarin (taken by mouth) — slowly prevents more clot formation; usually given for several months
- Direct thrombin inhibitors, such as fondaparinux (Arixtra)
- Fibrinolytic enzymes — help to dissolve a major clot. These include:
- Streptokinase
- Urokinase
- tPA
Surgery
In some cases, a filter may be placed in the inferior vena cava. The vena cava is a major vein. Blood from the lower body returns to the heart through this vein. The filter may trap any clots that break loose before it travels to the lungs.
If you are diagnosed with deep vein thrombosis, follow your doctor’s instructions.
Deep vein thrombosis – Prevention
General prevention measures include:
- Do not sit for long periods. If you are in a car or airplane or at a computer, get up often and move around.
- Do not smoke.
If you are admitted to the hospital, talk to your doctor about how to prevent blood clots, such as:
- Get out of bed and walk as soon as possible during your recovery.
- If you are restricted to bed:
- Do range of motion exercises in bed.
- Change your position at least every two hours.
- Wear compression stockings to promote venous blood flow.
- Use a pneumatic compression device. This device uses air to compress your legs and help improve venous blood flow.
- If prescribed by your doctor, take medication to reduce blood clots. This medication can reduce your chance of death due to blood clots.