Coronary angioplasty
(Balloon Angioplasty; Percutaneous Transluminal Coronary Angioplasty [PTCA]; Percutaneous Coronary Revascularization)
Coronary angioplasty – Definition
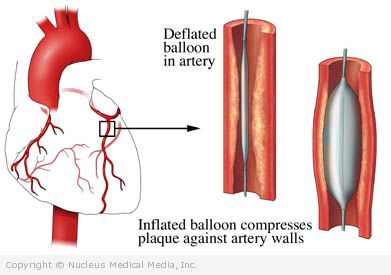
The insertion of a catheter carrying a balloon, through an artery in the groin or arm, into a blocked artery in the heart. The balloon is quickly inflated and deflated to open the artery to allow blood flow.
Coronary angioplasty – Reasons for Procedure
Atherosclerosis is a disease of the arteries. Cholesterol and fatty deposits build up on the walls of the arteries. This restricts blood flow. When this build up happens in the heart, it may lead to a heart attack. Lifestyle changes and medicines can be used to treat atherosclerosis. If they are not enough, an angioplasty may be done.
Coronary angioplasty – Possible Complications
If you are planning to have an angioplasty, your doctor will review a list of possible complications which may include:
- Bleeding at the point of catheter insertion
- Damage to the walls of arteries, causing you to need additional procedures or surgery
- Heart attack or arrhythmia (abnormal heart beats)
- Allergic reaction to x-ray dye
- Blood clot formation
- Infection
- Stroke
- Kidney failure (temporary)
Some factors that may increase the risk of complications include:
- Allergies to medicines, shellfish, or x-ray dye
- Obesity
- Smoking
- Bleeding disorder
- Age: 60 or older
- Recent pneumonia
- Recent heart attack
- Diabetes
- Kidney disease
Coronary angioplasty – What to Expect
Prior to Procedure
Your doctor will likely do the following:
- Blood tests — especially if you are taking certain medicines (high blood pressure pills, blood thinners, heart medicines)
- Electrocardiogram (ECG, EKG) — a test that records the heart’s activity by measuring electrical currents through the heart muscle
- Chest x-ray
In the days leading up to your procedure:
- Talk to your doctor about your current medicines. Certain medicines may need to be stopped before the procedure, such as:
- Anti-inflammatory drugs (eg, ibuprofen) for up to one week before surgery
- Blood-thinning medicines such as warfarin (Coumadin)
- Metformin (Glucophage) or glyburide and metformin (Glucovance)
- You should take aspirin before and during the procedure. Your doctor may also prescribe clopidogrel (Plavix) before the procedure.
- The night before, eat a light meal. Do not eat or drink anything after midnight.
- Arrange for a ride to and from the procedure.
- Arrange for help at home after returning from the hospital.
Coronary angioplasty – Anesthesia
Local anesthetic will be given. It will numb the area of the groin or arm where the catheter will be inserted. You will also be given sedation and pain medicine through an IV. This will help to keep you comfortable during the procedure.
Coronary angioplasty – Description of Procedure
The area of the groin or arm where the catheter will be inserted will be shaved, cleaned, and numbed. A needle will be inserted into the artery. You will receive blood thinning medicines during the procedure. A wire will be passed through the needle and into the artery. The wire will be guided through until it reaches the blocked artery in the heart. A soft, flexible catheter tube will then be slipped over the wire and threaded up to the blockage.
The doctor will be taking x-ray pictures during the procedure to know where the wire and catheter are. Dye will be injected into the arteries of the heart. This will make a better view of the arteries and blockages
Once the blockage is reached, a small balloon at the tip of the catheter will be rapidly inflated and deflated. This will stretch the artery open. The deflated balloon, catheter, and wire will be removed.
Your doctor may also insert a small mesh tube called a stent into the artery where there was a narrowing. A stent acts to keep the artery open by providing support inside the artery.
After the procedure is done and the blood thinning medicines have worn off, the catheter will be removed. Pressure will be applied for 20-30 minutes to control bleeding.
A bandage will be placed over the groin or arm area.
Coronary angioplasty – How Long Will It Take?
30 minutes to three hours
Coronary angioplasty – Will It Hurt?
The anesthetic should numb the area where the catheter is inserted. You may feel a burning sensation when the anesthesia is given. You may also feel pressure when the catheters are moved. Some people have a flushed feeling or nausea when the dye is injected. You may feel some chest pain during inflation of the balloon.
Coronary angioplasty – Average Hospital Stay
The usual length of stay is overnight. If the catheter is inserted in your arm or wrist, you may be able to go home the same day. Speak to your doctor to see if this is an option in your case.
Coronary angioplasty – Post-procedure Care
At the Hospital
You will likely need to lie still and flat on your back for a period of time. A pressure dressing may be placed over the area where the catheter was inserted to help prevent bleeding. Or, a vascular closure device may be used to seal the arterial puncture site. This will allow earlier movement and hospital discharge. It is important to follow the nurses’ directions.
At Home
- You may be sent home on blood-thinning therapy. This may include one or more of the following:
- Aspirin
- Warfarin
- Clopidogrel
- Prasugrel (Effient)
- Dabigatran etexilate (Pradaxa)
- Ice may help decrease discomfort at the insertion site. You may apply ice for 15-20 minutes each hour, for the first few days.
- To lower your risk for further complications of heart disease, you can make lifestyle changes. This includes eating a healthier diet, exercising regularly, and managing stress.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Be sure to follow your doctor’s instructions.
Sometimes the procedure is not successful or the artery narrows again. You may require repeat angioplasty or coronary artery bypass grafting (CABG).
Coronary angioplasty – Call Your Doctor
After you leave the hospital, contact your doctor if any of the following occurs:
- Signs of infection, including fever and chills
- Redness, swelling, increasing pain, excessive bleeding, or any discharge from the incision site
- Your arm or leg becomes painful, blue, cold, numb, tingly, swollen, or increasingly bruised
- Nausea and/or vomiting
- Pain that you cannot control with the medicines you have been given
- Cough, shortness of breath, or chest pain
- Joint pain, fatigue, stiffness, rash, or other new symptoms
In case of an emergency, call for medical help right away.