Cluster Headache
Cluster headaches – Definition
Cluster headache is a type of severe, recurring pain that is located on one side of the head. It received its name from the clustering, or pattern, of frequent headaches that usually occur.
There are two main types of cluster headaches:
- Episodic cluster headaches — These occur one or more times daily for 4-8 weeks. The headaches then enter a period of remission and come back months or years later.
- Chronic cluster headaches — These occur almost daily with headache-free periods lasting less than one month.
Either type of headache may convert to the other type.
Cluster headaches – Causes
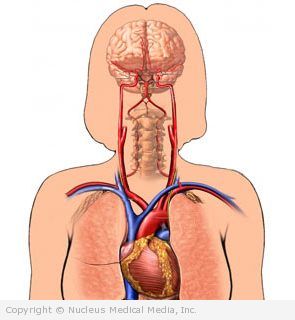
The cause of cluster headaches is unknown. It is thought that there is abnormal activation of the area of the brain responsible for regulating temperature, blood pressure, hormone release, and sleep. The pain is thought to be caused by a combination of widening of the blood vessels and inflammation of the nerves of the face.
Other possible causes include:
- Alcohol use
- Changes in barometric pressure
- Changes in sleep pattern
- Tobacco use
- Drugs, such as nitroglycerin
Cluster headaches – Risk Factors
Factors that increases your chance of cluster headaches include:
- Sex: males
- Age: 20-50 years old
- Prior head surgery or head injury
- Positive family history of cluster headaches
Cluster headaches – Symptoms
- Stabbing, penetrating, burning, or explosive head pain that:
- Has a rapid onset
- Is on one side of the head, but not both
- Often starts around the eye and spreads to the same side of the head
- Causes facial flushing
- Occurs daily or almost every day for 4-8 weeks
- Can occur 1-8 times per day
- Lasts 15 minutes to 3 hours
- Often occurs at about the same time each day
- Increases in intensity over time
- May start within two hours of going to sleep
- Can awaken you from sleep
- Aura — This can include visual disturbance, visual spots, or the inability to move one side of the body. This more often occurs with migraine. Auras can also happen with cluster headaches in a minority of cases.
- Restlessness and agitation
- Nausea
During the headache, other symptoms may occur on the affected side, including:
- Stuffy or runny nose
- Redness or watering of the eye on one side
- Droopy eyelid
- Constriction of the pupil of the eye
- Facial swelling and flushing, sweating
- Sensitivity to light and noise
Cluster headaches – Diagnosis
The doctor will ask about your symptoms and medical history. A physical and neurological exam will be done. A neurological exam tests the following:
- Mental status
- Cranial nerve functioning
- Motor and sensory functioning
- Coordination
- Reflexes
- Gait (walking)
The doctor will ask about the frequency and pattern of your headaches. To help provide answers, keep a diary of:
- When your headaches started and ended
- What you were doing at the time
- What you tried to relieve the pain
Tests are sometimes done to rule out other disorders. These tests may include:
- MRI scan — a test that uses magnetic waves to make pictures of structures inside the head
- CT scan of the brain — a type of x-ray that uses a computer to make pictures of structures inside the head
Cluster headaches – Treatment
Treatment aims to reduce the frequency of headaches and help relieve pain.
Lifestyle Changes and Self-care
- Maintain the same sleep routine. Avoid afternoon naps or sleeping in, which may bring on more headaches.
- Do not drink alcoholic beverages. Even a small amount of alcohol can trigger a headache during a cluster period.
- Learn stress management techniques. Stress can bring on a headache.
- Do not smoke. Tobacco may interfere with medicines.
- Find out what your triggers are and take steps to avoid them.
Medication
Drugs used to treat migraines often relieve acute attacks of cluster headaches. These drugs must be taken at the first sign of a headache.
Drugs used to treat cluster headaches include:
- Sumatriptan, zolmitriptan, or other triptans (given as an injection or nasal spray)
- Octreotide (given as an injection)
- Prednisone
- Lidocaine nose drops or spray
- Dihydroergotamine (eg, Migranal)
- Ergotamine (eg, Ergomar)
- Pain relievers with caffeine
- Glycerol (given as an injection into the nerve)—used when other treatments are ineffective
In some cases, the headache does not last long enough for drugs to be beneficial. Sometimes, the drugs just delay an attack, rather than stopping an attack.
Pain killers, especially narcotic drugs, should not be used during an acute attack.
Other medicines may be given to prevent or reduce the frequency of headaches. Examples of these drugs include:
- Intranasal civamide and capsaicin cream
- Steroid injections
- Verapamil (eg, Calan, Isoptin)
- Lithium (eg, Eskalith)
- Melatonin
- Valproate (eg, Depakote) or gabapentin (eg, Neurontin)
- Methysergide (eg, Sansert)
- Dihydroergotamine or a triptan
- Topiramate (eg, Topamax)
- Baclofen (eg, Lioresal)
- Beta-blockers
- Prednisone
- Clonidine (eg, Catapres-TTS)
- Amitriptyline (eg, Apo-Amitriptyline)
- Selective serotonin reuptake inhibitors (SSRIs)
Cluster headaches – Oxygen Therapy
Breathing 100% oxygen for 10-15 minutes often relieves cluster headache pain. The oxygen appears to decrease blood flow to the affected area of the brain. People under age 50 who have episodic cluster headaches seem to benefit most from oxygen therapy.
Oxygen therapy can be expensive, and there are risks with this therapy.
Surgery
As a last resort, some doctors may recommend cutting or destroying a facial nerve to eliminate pain.
Cluster headaches – Prevention
To prevent cluster headaches from getting worse, preventive medicine may be given. In addition:
- Maintain a regular sleep routine.
- If you smoke, quit.
- Avoid alcohol, narcotic analgesics, bright sunlight, and emotional stress.
- Get moderate physical exercise.
- Practice relaxation techniques.
- Take your medicine as directed.