Raynaud’s disease and phenomenon
Raynaud’s disease – Definition
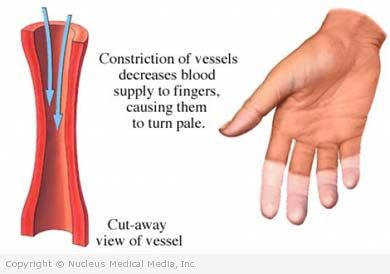
Raynaud’s disease and phenomenon are a problem with blood flow. During an attack, blood vessels narrow. This causes blood flow to the fingers and sometimes ears, nose, and lips to be severely reduced.
There are two types:
- Primary Raynaud’s (Raynaud’s Disease) — most common form, occurs by itself, in the absence of other medical conditions
- Secondary Raynaud’s (Raynaud’s Phenomenon) — more severe form, occurs in conjunction with other underlying medical conditions such as:
- Scleroderma
- Lupus
- Rheumatoid arthritis
- Sjogren’s syndrome
- Carpal tunnel syndrome
Raynaud’s disease – Causes
Blood vessels normally narrow with cold temperatures or emotional stress, such as excitement or nervousness. However, Raynaud’s is an abnormally exaggerated response.
It is not known what causes this abnormal reaction, but it is probably related to a problem of the sympathetic nervous system. Secondary Raynaud’s is believed to be caused by the associated disease.
Raynaud’s disease – Risk Factors
Factors that increased your risk of Raynaud’s syndrome include:
- Sex: female
- Age: 15 to 40 years old
- Jobs or leisure activities: Activities that subject the hands to repeated stress may increase the chance of developing Raynaud’s. For example:
- Typing
- Playing piano
- Regular operation of vibrating tools, as in construction
- Exposure to certain chemicals
- A connective tissue disease (such as scleroderma)
- Diseases of the arteries, including atherosclerosis
- Injuries to the hands or feet, such as wrist fractures or frostbite
- Smoking
- Certain medications, such as:
- Beta-blockers
- Cancer chemotherapy
- Cold remedies
- Migraine medications containing ergotamine
- Estrogen-containing medications
Raynaud’s disease – Symptoms
An attack of Raynaud’s may last a few minutes to a few hours. During an attack, symptoms may include:
- Skin discoloration–during an attack, skin color may change to white, blue, and red.
- White occurs when the arteries narrow or collapse.
- Blue appears when the fingers, toes, or other areas are not getting enough oxygen-rich blood.
- The skin turns red and may become swollen when the attack subsides and blood returns.
- Throbbing and tingling sensations, stinging, pain, and swelling of the affected area. This may occur at the end of the attack as blood flow returns to the area.
People with secondary Raynaud’s may experience other medical problems related to Raynaud’s, such as:
- Skin thinning and ulcerations
- Gangrene (tissue death)
- Many other symptoms related to their underlying connective tissue disorder
Raynaud’s disease – Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done. Tests may include:
- Nailfold capillaroscopy — study of the capillaries under a microscope
- Blood tests — to help distinguish between Raynaud’s disease and phenomenon, and to help identify underlying autoimmune conditions:
- Antinuclear antibody test (ANA)
- Erythrocyte sedimentation rate (ESR)
Raynaud’s disease – Treatment
There are several ways to reduce the symptoms of Raynaud’s during an attack:
Create Warmth for Fingers and Toes
- Run warm (not hot) water over fingers and toes as quickly as possible. However, do not place anything hot on your skin, as it may cause damage.
- If you are outside, move inside.
- Place your hands on a warm area of the body, such as under your armpits or on the abdomen.
Stimulate Blood Flow
Try to stimulate blood circulation by wiggling your fingers and toes, and making wide circles with your arms.
Medications
When the above measures fail, medications may help relieve symptoms. Medication may also help skin ulcers begin to heal. Medications may include:
- Calcium channel blockers, such as nifedipine (eg, Adalat, Procardia, Afeditab, Nifediac)
- Alpha-blockers, such as prazosin (eg, Minipress)
- Vasodilators, such as a nitroglycerin cream (eg, EMLA)
Surgery
Rarely, surgery may be done when symptoms are persistent and debilitating. This involves cutting the sympathetic nerves that supply the affected fingers. In extremely rare instances, a finger of toe that has suffered gangrene may require amputation.
Chemical Injection
Chemicals may be injected into the sympathetic nerve that is responsible for blood vessel constriction. The chemical stops the nerve.
Treating Underlying Medical Condition
If you have Raynaud’s phenomena, successful management of the underlying connective tissue or vascular disorder can help to relieve symptoms.
Raynaud’s disease – Prevention
There are no guidelines for preventing Raynaud’s disease and phenomenon. To prevent symptoms of Raynaud’s:
- Stay warm. Avoid cold temperatures when possible.
- Dress in layers.
- Always wear clothing that covers extremities (hats, gloves, socks, etc.).
- Learn to adapt to stressful situations.
- Avoid caffeine.
- Don’t smoke. If you smoke, quit.
- Exercise regularly.
- Consider using biofeedback training to control body temperature.
- Avoid the use of medications known to exacerbate Raynaud’s.
To minimize the risk of complications from Raynaud’s:
- Keep skin on fingers and toes lubricated and protected.
- Avoid injuries.