Iron-deficiency anemia
(Reduced Iron in Blood)
Iron-deficiency anemia – Definition
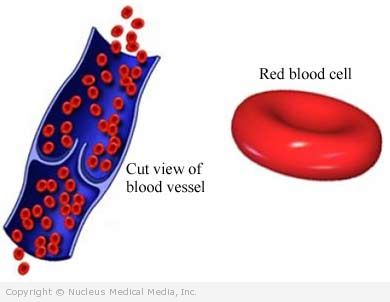
This condition results from reduced iron stores in the blood. This happens when you do not eat enough iron to replace the iron that your body uses. Your body uses iron to produce hemoglobin. This part of red blood cells carries oxygen to tissues and muscles. Bleeding a lot can also cause anemia.
Iron-deficiency anemia – Causes
Factors that play a role include:
- Iron that is poorly absorbed in the digestive tract (may occur due to intestinal diseases or surgery)
- Chronic bleeding (eg, heavy menstrual bleeding, bleeding in the gastrointestinal [GI] tract)
- Not enough iron in the diet (common cause in infants, children, and pregnant women)
Iron-deficiency anemia – Risk Factors
These factors increase your chance of developing this condition. Tell your doctor if you have any of these risk factors:
- Rapid growth cycles (infancy, adolescence)
- Heavy menstrual bleeding or chronic blood loss from the GI tract
- Pregnancy
- Diets that contain insufficient iron (rare in the United States)
- Breastfed infants who have not started on solid food after six months of age
- Babies who are given cow’s milk prior to age 12 months
- Alcoholism
Iron-deficiency anemia – Symptoms
While most people with mild anemia have no symptoms, when present, symptoms may include:
- Fatigue
- Pale skin
- Fingernail changes
- Weakness
- Headache
- Decreased work capacity
- Heart palpitations
- Infection
- Craving to eat things that are not food (called a pica), such as ice or clay
- Hair loss
- Shortness of breath during or after physical activity
Iron-deficiency anemia – Diagnosis
The doctor will ask about your symptoms and medical history, and perform a physical exam.
Tests may include:
- Serum iron
- Transferrin iron binding capacity
- Serum ferritin level
- Microscope examination of a blood smear
- Fecal occult blood test — to look for hidden blood in the stool
Iron-deficiency anemia – Treatment
Treatments may include:
Iron Supplements
Iron can be taken as a supplement or as part of a multivitamin. Iron comes in many “salt” forms. Ferrous salts are better absorbed than ferric salts. Ferrous sulfate is the cheapest and most commonly used iron salt. Slow-release or coated products may cause less stomach problems. However, they may not be absorbed as well. Some products contain vitamin C to improve absorption. Talk to your doctor, though, because your iron level could get too high.
Iron-Fortified Cereal
Your doctor may recommend that you feed your baby iron-fortified cereal.
Iron-deficiency anemia – Prevention
To help reduce you or your child’s chances of getting this condition, take the following steps:
- Eat a diet rich in iron (eg, oysters, meat, poultry, fish)
- Avoid foods that interfere with iron absorption, like black tea
- Ask your doctor if your infant is getting enough iron — The general guidelines are:
- Starting at four months, breastfed infants need an iron supplement until they get enough iron from other sources, like infant cereal or iron-fortified formula.
- Bottle-fed infants should get a formula that is fortified with iron.
- Many premature infants need extra iron starting at one month of age.
