Asthma – Child
Asthma – Child – Definition
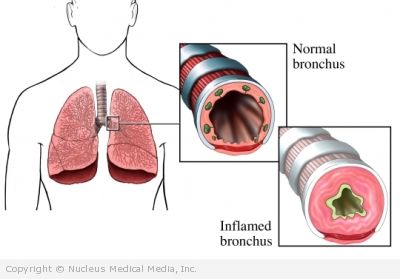
Air travels in and out of the lungs through bronchial tubes. Asthma is a chronic inflammation of these tubes. This inflammation causes airways to narrow. This makes it hard to breath. There are different degrees of asthma. Some people may have very mild asthma with rare flare-ups. Others may have a severe, constant asthma.
Asthma is the most common chronic disease found in children. If your child is having trouble breathing, call 911 immediately. This is a potentially serious condition that needs immediate medical attention.
If it is not an emergency, but you suspect your child may have asthma, contact your doctor. With proper treatment, asthma can be controlled.
Asthma – Child – Causes
The exact causes of asthma are unknown. It is thought that a mix of genes and environment causes asthma. Possible causes include:
- Family history
- Tendency to develop allergies
- Respiratory infections
- Contact with allergens when immune system is developing
Certain conditions are known to trigger an asthma attack. These include:
- Exercise — especially in cold air
- Tobacco smoke
- Substances that cause allergies (allergens)
- Dust
- Food — peanuts, milk, wheat, eggs, and tree nuts are common
- Mold
- Animal hair
- Respiratory infection
- Abrupt change in weather
Asthma – Child – Risk Factors
These factors increase your child’s chance of asthma. Tell your doctor if your child has any of these risk factors:
- Family history
- Tendency to develop allergies
- History of respiratory infections
- Exposure to tobacco smoke
- Premature birth
- History of allergies and/or eczema
- Chlorinated pool use in children who are already at risk for asthma
- Taking medicines such as acetaminophen
Asthma – Child – Symptoms
If your child has any of these symptoms do not assume it is due to asthma. These may be caused by other conditions. Tell your doctor if your child has any of these:
- Shortness of breath
- Coughing
- Trouble breathing
- Wheezing
- Chest tightness
- Fatigue
- Child complains of chest pain or odd sensations
- Difficulty during feeding in infants
- Trouble sleeping
- Child avoids exercise or sports
Asthma – Child – Diagnosis
Your doctor will ask about you about your child’s symptoms and medical history. A physical exam will be done. The doctor will listen to your child’s lungs. Your doctor may refer you to a specialist. A pulmonologist focuses on the lungs. An immunologist focuses on allergies.
Tests may include the following:
- Spirometry test — test that measures how well your child breaths; your child will be asked to take deep breaths and then exhale into a tube that is hooked to a machine
- Challenge test — test that uses spirometry to measure how well your child breaths after causing asthma symptoms
- Pulse oximetry — test that uses a sensor on a finger to measure oxygen concentration
- Medication — in young children unable to undergo spirometry testing, the doctor may prescribe a bronchodilator medication (drug that opens airways); if your child’s symptoms get better then the doctor may diagnose asthma
- X-ray — test that uses radiation to form an image; chest x-ray used to rule out infection and disease
- Skin testing — test that introduces very small amounts of common allergens into the skin; used to identify common allergens that may trigger asthma symptoms
Asthma – Child – Treatment
Talk with your child’s doctor about the best plan for your child. You and your child’s doctor should also create an asthma action plan. This is a plan your child will follow to help control his asthma and handle asthma attacks. Treatment will vary based on how many asthma episodes your child has and any specific symptoms. Treatment options include the following:
Lifestyle Changes
You can help your child reduce his chance of triggering an asthma attack by making lifestyle changes, such as:
- Know what your child is allergic to and avoid known triggers. These may include certain foods, pollen, and air pollution.
- Avoid having your child be exposed to tobacco smoke.
- Have proper heating, cooling, and ventilation systems in your home.
Medications
Medications used to treat asthma fall into one of two categories:
- Quick relief medications — These are also sometimes called rescue medications and are used to quickly treat breathing difficulties. Common inhalers include:
- Albuterol
- Levalbuterol
- Ipratropium
- Pirbuterol
- Long-term control:
- Inhaled corticosteroids
- Systemic corticosteroids
- Long-acting beta agonist — in most cases, prescribed with an inhaled corticosteroid
- Leukotriene modifiers such as montelukast (Singulair) and zafirlukast (Accolate)
- Theophylline
- Cromolyn or nedocromil
- Zileuton (Zyflo), a 5-lipoxygenase inhibitor
- Combination medications that include a long-acting bronchodilator and an inhaled corticosteroid
In addition to the medicines, children older than six months should get a yearly flu shot. Children with asthma are at a higher risk of having complications from the flu.
Allergy Shots (Immunotherapy)
Your child’s asthma may be triggered by allergies. In this case, your doctor may recommend allergy shots. These shots are very small amounts of an allergen injected into the skin. Over time your child will react less to the specific allergen(s). With less triggers the asthma also decreases.
Asthma – Child – Prevention
There are no known ways to prevent your child from developing asthma. If you child already has asthma, you can reduce your child’s risk of asthma episodes by helping him to follow the treatment plan.