Systemic Lupus Erythematosus
(Lupus; SLE; Lupus, Systemic)
Lupus – Definition
Lupus is an autoimmune disease. It inflames:
- Joints
- Tendons
- Skin
- Other connective tissue and organs
It causes the immune system to make antibodies that attack the body’s healthy cells and tissue.
Lupus – Causes
The cause of lupus is unknown. Researchers believe it may be a combination of:
- Genetic factors
- Environmental factors, which may include:
- Sunlight (UV rays)
- Stress
- Viral or other type of infection
- Drug-induced ( methyldopa, procainamide, hydralazine, isoniazid, chlorpromazine, TNF-blocking drugs)
Lupus – Risk Factors
These risk factors increase your chance of developing lupus. Tell your doctor if you have any of these risk factors:
- Sex: female to male ratio: 10:1
- Age: childbearing age (20-45 years)
- Race: African American, Native American, Asian, and Hispanic
Lupus – Symptoms
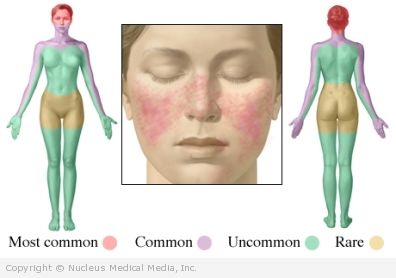
Symptoms can be mild or very severe. For some people, only part of the body (eg, skin) is affected. For others, many parts are affected. Though symptoms can be chronic, they can flare up and get better on and off.
Common symptoms:
- Swollen and/or painful joints
- Fever
- Skin rashes over areas exposed to sunlight (especially on the nose and cheeks)
- Extreme fatigue
Other symptoms may include:
- Hair loss
- Chest pain, coughing up blood, shortness of breath, difficulty breathing
- Kidney inflammation
- High blood pressure
- Anemia or other blood disorders
- Sensitivity to sunlight
- Raynaud’s phenomenon
- Ulcers in nose or mouth
- Swollen glands
- Headaches
- Dizziness
- Seizures
- Stroke
- Inflamed heart, heart vessels, or membrane surrounding the heart
- Blood clots
A pregnant woman who has lupus may experience complications, like a flair-up of symptoms, high blood pressure, and kidney inflammation. There may also be problems with the pregnancy (eg, premature birth, miscarriage, restricted growth in the fetus).
Lupus – Diagnosis
Diagnosing lupus can be difficult. It can take time to identify the condition because you may develop more symptoms over time.
To aid in making the diagnosis, the American College of Rheumatology (ACR) has created the following criteria. You must have 4 out of the 11 items to be diagnosed with lupus:
- Butterfly facial rash
- Rash (or red patches) on sun-exposed areas
- Skin photosensitivity (easily burned by the sun)
- Ulcers in the mouth or near the throat
- Arthritis in at least two joints
- Inflammation of the lining of the heart or lungs (called serositis)
- Kidney problems (identified by kidney function tests)
- Seizures or psychosis that are not caused by another condition
- Abnormally low number of blood cells
- Antinuclear antibodies — These are immune chemicals produced by your body that attack the nuclei in your cells. These antinuclear antibodies may contribute to the cause of lupus.
- Immune dysfunction — In people with lupus, several other antibodies have been found. These antibodies can be detected with lab tests.
To find out if you do meet the criteria, your doctor will order tests, such as:
- Blood tests, such as complete blood count, antinuclear antibody (ANA) test
- Urine test to check kidney functioning
- Imaging tests (eg, MRI scan) if you have neurological symptoms
Depending on your symptoms, your doctor may diagnosis you with lupus even if you have less than four of the ACR’s criteria.
Your doctor will also rule out other conditions that may have similar symptoms, such as:
- Sjogren syndrome (an inflammatory disease)
- Fibromyalgia
- Idiopathic thrombocytopenic purpura (a blood disorder)
- Rheumatoid arthritis
Lupus – Treatment
Treatment options depend on your symptoms.
Medication
There are many different kinds of medicines that are used to treat lupus. Examples include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) — to relieve joint pain
- Antimalarial drugs (eg, hydroxychloroquine, chloroquine) — to relieve joint pain, fatigue, and rashes
- Corticosteroids — to reduce inflammation
- Drugs to suppress the immune system (eg, azathioprine, mycophenolate, methotrexate) — to help with symptom relief if the other medicines are not working
- Prescription steroid cream for rashes (eg, fluocinonide cream)
- Hormonal medicine ( dehydroepiandrosterone [DHEA]) — to reduce symptoms
- B-cell therapy (eg, rituximab) — experimental medicine to reduce the number of white blood cells
Your doctor may recommend that you take a combination of medicines.
Medicines for severe symptoms include:
- Oral and intravenous corticosteroids to control and limit inflammation in kidney, brain, lung, and heart, as well as in cases of severe anemia
- Immunosuppressive drugs to suppress the body’s autoimmune system
- Mycophenolate, azathioprine, and cyclophosphamide for kidney disease or other life- or organ-threatening conditions
- Rituximab for refractory disease
Other Treatment Options
In addition to taking medicine, your doctor may recommend that you:
- Eat a healthy diet. Adding omega-3 fatty acids, found in certain types of fish, may help with symptoms.
- Exercise regularly. Your doctor can give you advice as to which exercises are safe for you to do.
- Protect your skin from the sun. Wear sunscreen with an SPF of at least 30 whenever you go out in the sun.
- Work with a therapist. Counseling may help you to build skills to cope with your condition.
Lupus – Prevention
You cannot prevent lupus because the cause is unknown.
To prevent flare-ups of symptoms:
- Schedule regular check-ups.
- Treat any and all infections quickly and vigorously.
- Avoid sun exposure and wear sunscreen and protective clothing when outdoors.
- Eat a healthful diet, one that is low in saturated fat and rich in whole grains, fruits, and vegetables .
- Limit emotional stress.
- Get adequate rest.
- Exercise moderately (as much as your condition allows) with your doctor’s permission.
- Call your doctor if you think you will have a flare-up.
- Avoid oral contraceptives, especially if you have had a blood clot.