Coronary artery disease
(CAD; Coronary Atherosclerosis; Silent MI; Coronary Heart Disease; Ischemic Heart Disease; Atherosclerosis of the Coronary Arteries)
Coronary artery disease – Definition
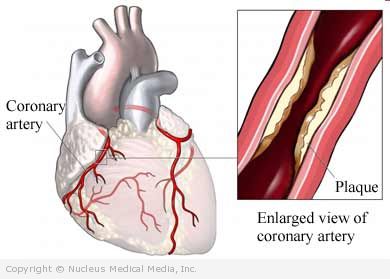
Coronary arteries bring oxygen rich blood to the heart muscle. Coronary artery disease (CAD) is blockage of these arteries. If the blockage is complete, areas of the heart muscle may be damaged. In severe case the heart muscle dies. This can lead to a heart attack, also known as a myocardial infarction (MI).
Coronary artery disease is the most common form of heart disease. It is the leading cause of death worldwide.
Coronary artery disease – Causes
Causes include:
- Thickening of the walls of the arteries feeding the heart muscle
- Accumulation of fatty plaques within the coronary arteries
- Sudden spasm of a coronary artery
- Narrowing of the coronary arteries
- Inflammation within the coronary arteries
- Development of a blood clot within the coronary arteries that blocks blood flow
Coronary artery disease – Risk Factors
Major risk factors include:
- Sex: male (men have a greater risk of heart attack than women)
- Age: 45 and older for men, 55 and older for women
- Heredity: strong family history of heart disease
- Obesity and being overweight
- Smoking
- High blood pressure
- Sedentary lifestyle — Poor fitness can also increase your risk of CAD and premature death.
- High cholesterol (specifically, high LDL cholesterol, and low HDL cholesterol)
- Diabetes
- Metabolic syndrome (combination of high blood pressure, abdominal obesity, and insulin resistance)
Other risk factors may include:
- Stress
- Excessive alcohol use
- Depression
- A diet that is high in saturated fat, trans fat, cholesterol, and/or calories — Drinking sugary beverages on a regular basis may increase your risk of CAD.
Coronary artery disease – Symptoms
CAD may progress without any symptoms.
Angina is chest pain that comes and goes. It often has a squeezing or pressure-like quality. It may radiate into the shoulder(s), arm(s), or jaw. Angina usually lasts for about 2-10 minutes. It is often relieved with rest. Angina can be triggered by:
- Exercise or exertion
- Emotional stress
- Cold weather
- A large meal
Chest pain may indicate more serious unstable angina or a heart attack if:
- It is unrelieved by rest or nitroglycerin
- Severe angina
- Angina that begins at rest (with no activity)
- Angina that lasts more than 15 minutes
Accompanying symptoms may include:
- Shortness of breath
- Sweating
- Nausea
- Weakness
Immediate medical attention is needed for unstable angina. CAD in women may cause less classic chest pain. It is likely to start with shortness of breath and fatigue.
Coronary artery disease – Diagnosis
If you go to the emergency room with chest pain, some tests will be done right away. The tests will attempt to see if you are having angina or a heart attack. If you have a stable pattern of angina, other tests may be done to determine the severity of your disease.
The doctor will ask about your symptoms and medical history. A physical exam will be done.
Tests may include:
- Blood tests — to look for certain substances in the blood called troponins which help the doctor determine if you are having a heart attack
- Electrocardiogram (ECG, EKG) — records the heart’s activity by measuring electrical currents through the heart muscle, and can reveal evidence of past heart attacks, acute heart attacks, and heart rhythm problems
- Echocardiogram — uses high-frequency sound waves (ultrasound) to examine the size, shape, and motion of the heart, giving information about the structure and function of the heart
- Exercise stress test — records the heart’s electrical activity during increased physical activity
- Nuclear stress test — the heart is observed while exercising and radioactive material highlights impaired blood flow to help locate problem areas
- Coronary calcium scoring — a type of x-ray called a CAT scan that uses a computer to look for the presence of calcium in the heart arteries
- Coronary angiography — x-rays taken after a dye is injected into the arteries to allows the doctor to look for abnormalities in the arteries
Coronary artery disease – Treatment
Treatment may include:
Nitroglycerin
This medicine is usually given during an attack of angina. It can be given as a tablet that dissolves under the tongue or as a spray. Longer-lasting types can be used to prevent angina before an activity known to cause it. These may be given as pills or applied as patches or ointments.
Blood-Thinning Medications
A small, daily dose of aspirin has been shown to decrease the risk of heart attack. Ask your doctor before taking aspirin daily.
Other blood-thinning medicines include:
- Warfarin (Coumadin)
- Ticlopidine (Ticlid)
- Clopidogrel (Plavix)
- Prasugrel (Effient)
Beta-Blockers, Calcium-Channel Blockers, and ACE-Inhibitors
These may help prevent angina. In some cases, they may lower the risk of heart attack.
Medications to Lower Cholesterol
Medicines, like statins, are often prescribed to people who have CAD. Statins (eg, atorvastatin [Lipitor]) lower cholesterol levels, which can help to prevent CAD events.
Revascularization
Patients with severe blockages in their coronary arteries may benefit from procedures to immediately improve blood flow to the heart muscle:
- Percutaneous coronary interventions (PCI) — such as balloon angioplasty, in some cases, a wire mesh stent is placed to hold the artery open
- Coronary artery bypass grafting (CABG) — segments of vessels are taken from other areas of the body and are sewn into the heart arteries to reroute blood flow around blockages
Some studies have shown that CABG may be more effective than PCI. Lifestyle changes and intensive medicine may also be just as effective as PCI.
Options for Refractory Angina
For patients who are not candidates for revascularization procedures but have continued angina despite medicine, options include:
- Enhanced external counterpulsation (EECP) — large air bags are inflated around the legs in tune with the heart beat. The patient receives 5 one-hour treatments per week for seven weeks. This has been shown to reduce angina and may improve symptom-free exercise duration.
- Transmyocardial revascularization (TMR) — surgical procedure done with laser to reduce chest pain.
- Researchers are also studying gene therapy as a possible treatment.
Coronary artery disease – Prevention
To reduce your risk of getting coronary artery disease:
- Maintain a healthy weight.
- Eat a heart healthy diet that is low in saturated fat, red meat and processed meats, and rich in whole grains, fruits, and vegetables.
- Begin a safe exercise program with the advice of your doctor.
- If you smoke, quit.
- Treat your high blood pressure and/or diabetes.
- Treat high cholesterol or triglycerides.
- Ask your doctor about taking a low-dose aspirin every day.
- In certain patients, taking rosuvastatin (Crestor) may be another option. Talk to your doctor.