Myoclonus – Definition
Myoclonus is a brief and rapid twitching of a muscle or muscle groups. The twitching or jerking happens suddenly. It cannot be stopped or controlled at will.
There are different types. Some occur normally, like the hiccups or a movement while falling asleep. Other types are abnormal. The condition is classified according to:
- Underlying cause
- Pattern of movement
- Origin within the body
Myoclonus – Causes
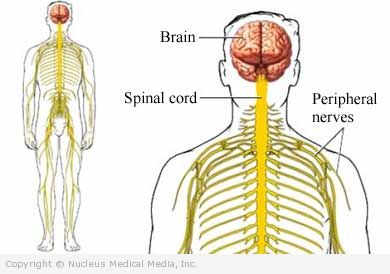
The movements are caused by an abnormal electrical discharge in the nervous system. The electrical discharge may originate in the:
- Brain
- Spinal cord
- Nerve in the body
The message travels along the nerves to the muscle. The nerve stimulates a muscle or group of muscles to suddenly contract.
The exact mechanism triggering the abnormal electrical discharge depends on the cause. Myoclonus is often a symptom of a nervous system or metabolic condition. Possible causes include:
- A lack of oxygen or nutrients
- Certain medications or toxins
- Nervous system disorders, such as:
- Head or spinal cord trauma or injury
- Tumors of the brain or spinal cord
- Multiple sclerosis
- Parkinson’s disease
- Alzheimer’s disease
- Creutzfeldt-Jakob disease
- Huntington’s disease
- Encephalitis
- Stroke
- Epilepsy
- Coma
- Paraneoplastic syndromes (disorders that happen in people with certain types of cancer)
- Metabolic disorders, such as:
- Lipid storage disease (a congenital disorder that usually occurs in children)
- Electrolyte imbalance
- Respiratory failure
- Liver failure
- Kidney failure
- Malabsorption syndromes, such as Whipple’s disease or celiac disease
Myoclonus – Risk Factors
A family history of myoclonus is the only common risk factor that has been identified.
Myoclonus – Symptoms
Myoclonic symptoms vary from mild to severe. This depends on the cause of the problem. It may begin in childhood or adulthood. The unexpected jerking or twitching may occur once in a while or often. It may be limited to one region of the body or affect all muscle groups.
Light, sound, touch, or movement may be triggers. Or, it may happen for no clear reason. Movements can occur at rest or during other movements. There may be one or a series of twitches. Sometimes the jerking occurs in a pattern. Other times there is no pattern. Myoclonus can become so severe that it interferes with eating, speaking, or walking.
Myoclonus – Diagnosis
Your doctor will ask about your symptoms and medical history. She will also do a physical exam. Your doctor will try to determine the following:
- The origin in the nervous system of the myoclonus
- If an underlying condition is responsible for the symptoms
Tests may include:
- Electroencephalogram (EEG) — a test that records the brain’s activity by measuring electrical currents through the brain
- Electromyogram (EMG) — a test that measures and records the electrical activity of the muscles
- MRI scan — a test that uses magnetic and radio waves to take pictures of the inside of the body
- CT scan — a type of x-ray that uses a computer to make pictures of the inside of the body
- Blood tests—may include:
- Thyroid function
- Blood chemistry
- Complete blood cell count
- Toxicology screen to check for drugs or toxins
- Blood tests looking for other metabolic causes
- Single photon emission computed tomography (SPECT) — a test that takes pictures of the inside of the body and displays them on a computer screen
Myoclonus – Treatment
Treatment aims to reduce how severe the involuntary movements are. The drugs given depend on the underlying cause. In some case, multiple drugs are needed to reduce twitching. Some have serious side effects.
- Sedatives:
- Lorazepam (Ativan)
- Diazepam (Valium)
- Clonazepam (Klonopin)
- Piracetam
- Tetrabenazine
- Anticonvulsants:
- Clonazepam (Klonopin)
- Divalproate sodium (Depakote)
- Gabapentin (Neurontin)
- Topiramate (Topamax)
- Primidone (Myidone, Mysoline)
- Carbamazepine (Tegretol)
- 5-hydroxytryptophan (5-HTP)
- Adrenocorticotropic hormone (ACTH)
Myoclonus – Prevention
Taking these steps may help to reduce your chance of myoclonus:
- Brain injury — Take care to prevent accidents or injury. For example, wear a helmet when riding a bicycle or motorcycle.
- Medication side effects — If twitching begins after starting a new medication, tell your doctor. Your doctor may be able to lower the dose or switch to a different medication.