Colon cancer – Definition
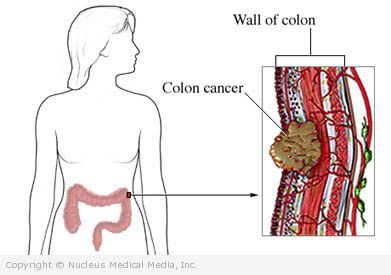
Colon cancer is the growth of cancer in the large intestine.
Cancer occurs when cells in the body divide out of control or order. If cells keep dividing, a mass of tissue, called a growth or tumor, forms. The term cancer refers to malignant tumors. They can invade nearby tissue and spread to other parts of the body.
Colon cancer – Causes
The cause of colon cancer is unknown.
Colon cancer – Risk Factors
Research shows that certain risk factors are associated with colon cancer:
- Age: 50 or older
- Diets high in fat, low in fiber
- History of polyps (benign growths) in the colon and rectum
- Hereditary conditions such as familial polyposis or Lynch syndrome
- Personal history of colorectal cancer
- Family history of colon or rectal cancer, especially a parent, sibling, or child
- History of ulcerative colitis (inflammation of the lining of the colon) or Crohn’s disease
- Other risk factors include:
- Obesity
- High body mass index (BMI)
- Physical inactivity
- Diabetes
- Smoking
- Heavy alcohol intake
- Diet high in red meats and low in fish
Colon cancer – Symptoms
Colon cancer often does not have any symptoms, but some symptoms associated with colon cancer include:
- A change in bowel habits such as diarrhea, constipation, or feeling that the bowel does not empty completely — lasting for more than a few days in people aged 50 and older
- Blood (either bright red or very dark) in the stool
- Stools that are narrower than usual
- Abdominal discomfort (frequent gas pains, bloating, fullness, and/or cramps)
- Unexplained weight loss
- Feeling tired frequently
- These may also be caused by other, less serious health conditions. Anyone experiencing these symptoms should see a doctor.
Colon cancer – Diagnosis
The doctor will ask about your symptoms and medical history. A physical exam will be done.
Tests to screen for cancer or precancerous polyps include:
- Digital rectal exam — use of a doctor’s gloved finger to examine the rectum for lumps or growths
- Fecal occult blood test — a test to check for hidden blood in the stool
- Colonoscopy — examination of the rectum and entire colon using a lighted tube called a colonoscope
- Sigmoidoscopy — an examination of the lower colon using a lighted tube called a sigmoidoscope
- Barium enema — a rectal injection of barium given to coat the lining of the colon and rectum; done before x-rays, in order to create better image of the lower intestine
- CT colonography — a radiology test that looks at your large intestines
Additional tests may be done to confirm the presence of cancer, determine what stage the cancer is in and/or determine if the cancer has spread:
- Biopsy — the removal of colon or rectal tissue to be tested for cancer
- Polypectomy — the removal of a polyp during a sigmoidoscopy or colonoscopy
- Blood tests to look for anemia and markers of cancer in the blood
- CT scan — a type of x-ray that uses a computer to make pictures of structures inside the body; to identify the spread of the tumor outside the colon
- PET/CT scan — a test that produces images showing the amount of functional activity in tissue being studied; it helps in finding out if the disease has spread outside the pelvis to other organs
- Transrectal ultrasound — an ultrasound probe that is inserted into the rectum sends out sound waves to image the tumor
Colon cancer – Treatment
Treatment depends on the stage of the cancer but may include:
Surgery
Surgery is the main treatment. It requires removal of the cancerous tumor and nearby colon tissue. Depending on the size and location of the tumor the surgery may be done by:
- Laparoscopy — removal of early stage cancer.
- Open surgery — to remove tumors, colon tissue and potentially nearby lymph nodes. The surgeon will also look for additional cancer in the colon during the surgery.
In some cases, the tumor and nearby healthy colon tissue will be removed. Healthy tissue is removed in case the cancer has begun to spread. The removal of a part of the colon is called a hemicolectomy. In most cases, the remaining healthy portions of the colon are reconnected. Sometimes, the end of the healthy colon is temporarily or permanently attached to an opening in the abdomen. This is called a colostomy. It allows body waste to pass out of the body if the colon can not do so.
Radiation Therapy
This is the use of radiation to kill cancer cells and shrink tumors. It is directed at the site of the tumor from a source outside the body. This therapy is aimed at the immediate area of the cancer.
Chemotherapy
This therapy uses drugs to kill cancer cells. It may be given in many forms, including pill, injection, and via a catheter. The drugs enter the bloodstream and travel through the body killing mostly cancer cells. It can also kill some healthy cells. This therapy is systemic meaning it affects your entire body.
If you are diagnosed with colon cancer, follow your doctor’s instructions.
Colon cancer – Prevention
Screening
The cause of most cancers are not known. However, it is possible to prevent many colon and rectal cancers by finding and removing polyps that could become cancerous. Beginning at age 50, both men and women at average risk for the development of colon and rectal cancer should follow one of the five screening options listed below:
- Yearly fecal occult blood test or fecal immunochemical test
- Colonoscopy every 10 years
- Flexible sigmoidoscopy every five years
- Double contrast barium enema (x-rays of the colon and rectum) every five years
- CT colonography every five years
Be sure to discuss these cancer screening tools with your doctor to see which option is best for you.
People with any of the following risk factors should begin colon and rectal cancer screening at age 40 or earlier and/or undergo screening more often:
- Strong family history of colon or rectal cancer or polyps
- Known family history of hereditary colon or rectal cancer syndromes
- Personal history of colon and rectal cancer or adenomatous polyps
- Personal history of chronic inflammatory bowel disease
Lifestyle Changes
There are also lifestyle changes that may reduce your risk of colon cancer, such as:
- Not smoking
- Being physically active (eg, exercising at least 30 minutes on most days of the week)
- Maintaining a healthy weight
- Eating a high-fiber diet — Fiber is found in all plant foods (eg, fruits, veggies, grains, and legumes). Fiber from cereals and whole grains may be especially helpful in reducing your risk of colon cancer.
- Making other changes to your diet, like eating plenty of fruits and vegetables, not eating a lot of red meat, and not abusing alcohol