Cirrhosis – Definition
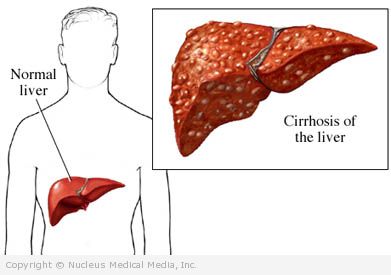
Cirrhosis is a disease in which the liver becomes permanently damaged and the normal structure of the liver is changed. Healthy liver cells are replaced by scarred tissue. The liver is not able to do its normal functions, such as detoxifying harmful substances, purifying blood, and making vital nutrients. In addition, scarring slows down the normal flow of blood through the liver, causing blood to find alternate pathways. This may result in gastric or esophageal varices.
Cirrhosis – Causes
Causes of cirrhosis include:
- Excessive consumption of alcohol
- Hepatitis C, B, and D
- Autoimmune hepatitis
- Inherited diseases:
- Glycogen storage disease
- Galactosemia
- Fructose intolerance
- Tyrosinemia
- Hemochromatosis
- Wilson’s disease
- Alpha1-antitrypsin deficiency
- Cystic fibrosis
- Nonalcoholic steatohepatitis (NASH), associated with:
- Diabetes
- Obesity
- Heart disease
- High blood triglycerides
- Steroid use
- Bile duct blockages, associated with:
- Cirrhosis
- Congenital defects
- Scarred ducts — sometimes related to inflammatory bowel disorders
- Gallbladder surgery
- Pancreatitis
- Drugs and toxins:
- Arsenic
- Isoniazid
- Methotrexate
- Excess vitamin A
- Infections:
- Schistosomiasis
- Brucellosis
- Echinococcosis
- Advanced or congenital syphilis
- Heart failure, causing blood to repeatedly back up into the liver
Cirrhosis – Risk Factors
A risk factor is something that increases your chance of getting a disease or condition. Risk factors include:
- Alcohol abuse
- Hepatitis infection
- Use of drugs toxic to the liver
- Being overweight or gaining weight
- Diabetes that is poorly controlled
- Ingestion of too much iron
Cirrhosis – Symptoms
Cirrhosis often does not cause symptoms early in the disease process. Symptoms start when the liver begins to fail, as scar tissue replaces healthy cells. Symptom severity depends on the extent of liver damage.
Early symptoms include:
- Fatigue
- Poor appetite
- Abdominal swelling, tenderness, and pain
- Nausea
- Weight loss
- Weakness
- Enlarged breasts in men
Later symptoms, some due to complications, include:
- Yellowing of the skin or eyes ( jaundice)
- Reddened palms
- Loss of body hair
- Shrunken testicles
- Enlarged liver
- Enlarged spleen
- Appearance of thin, purplish-red, spidery looking blood vessels on the skin, especially around the navel
- Dark urine
- Water retention and swelling in the legs and abdomen
- Bleeding and bruising
- Vomiting blood
- Itching
- Menstrual problems
- Abdominal infections
- Impotence
- Forgetfulness
- Confusion
- Agitation
- Tremors
- Coma
- Inability to fully process drugs
- Enlarged, twisted, thin-walled blood vessels called varices that bleed easily and sometimes catastrophically (usually located in the esophagus)
- Liver cancer
- Osteoporosis
- Gallstones
- Arrhythmias
- Sleep disturbances
- Ulcers
- Breathing problems
- Insulin resistance
Cirrhosis – Diagnosis
The doctor will ask about your symptoms and medical history and perform a physical exam.
Tests may include:
- Blood tests — to assess how well the liver is working and determine a cause
- CT scan, ultrasound, or liver/spleen scan — to identify changes in the liver
- Liver biopsy — analyzing a sample of liver tissue removed via a thin needle inserted through the abdomen and into the liver
- Laparoscopy — looking at the liver via a thin tube with a lighted tip inserted through a small incision near the belly button
Other tests may include:
- Inserting a catheter into the liver vein and measuring the pressure within that vein; rarely necessary
- Removing fluid from the abdomen and examining it
- Other tests to determine what caused the cirrhosis and what complications may occur
Cirrhosis – Treatment
There is no cure for cirrhosis. The goals of treatment are to keep the condition from getting worse, including:
- Control the cause
- Treat underlying medical conditions
- Prevent additional damage
- Treat symptoms and complications
- Liver cancer screenings
Treatments include:
Medication
Doctors prescribe drugs to:
- Treat hepatitis and complications that arise
- Reduce the absorption of waste products and toxins in the digestive system
- Reduce the risk of a blood vessel breaking
- Fight infections
- Shed excess fluids
Surgery
Liver transplant — may be done if:
- Complications can no longer be controlled using medical therapy.
- The liver stops functioning.
Endoscopy — This is used to tie off bleeding blood vessels (varices) or to inject drugs to cause clotting. A thin tool with a lighted tip is inserted down the throat to help the doctor see and access the varices, which are located in the esophagus.
Self-care
- Stop drinking alcohol completely.
- Do not take any medicines without your doctor’s approval, including over-the-counter drugs.
- Eat a balanced diet. Choose a variety of fruits and vegetables, as well as lean proteins, like beans and poultry.
- If your liver disease is more advanced, you may need to limit protein intake, because your weakened liver will not be able to process it properly.
- You may need to limit salt in your diet, because it increases water retention.
- Take any vitamin supplements your doctor recommends.
- Put your feet and legs up to decrease swelling.
- Due to increased risk of infections, doctors recommend:
- Getting vaccines for flu, pneumonia, and hepatitis
- Avoiding raw seafood
- Avoiding people who sick with communicable diseases, like the flu or cold
- Washing your hands often
If you are diagnosed with cirrhosis, follow your doctor’s instructions.
Cirrhosis – Prevention
To decrease the risk of cirrhosis:
- Drink alcohol in moderation. Moderate alcohol intake is no more than two drinks per day for men and one drink per day for women.
- Get hepatitis vaccines.
- Practice safe sex to lower your chance of getting hepatitis B.
- If you use IV drugs, do not share needles, which can spread hepatitis B, C, or D.
- Maintain a healthy weight.
- Follow your doctor’s recommendations about blood tests when taking medications that may damage the liver.