(Unstable Angina; Stable Angina; Angina Pectoris; Cardiac Angina; Variant Angina)
Angina – Definition
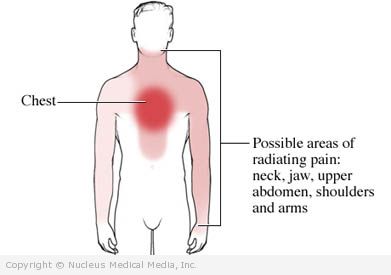
Angina is a pain or discomfort in the chest. It often has a squeezing or pressure-like feel. This discomfort can also be felt in the shoulders, arms, neck, jaws, or back. Anginal pain usually lasts for no more than 2-10 minutes. It is relieved by rest or nitroglycerin.
Types of angina include:
- Stable angina — has a predictable pattern. You generally know what brings it on and relieves it. You may also know what the intensity will be.
- Unstable angina — is more unpredictable or severe. Chest pain may occur while resting or even sleeping (nocturnal angina). The discomfort may last longer and be more intense than that of stable angina.
- Unstable angina may be a sign that you are about to have a heart attack. It should be treated as an emergency.
- Variant or prinzmetal’s angina — occurs when you are at rest. It most often occurs in the middle of the night. It can be quite severe.
Angina – Causes
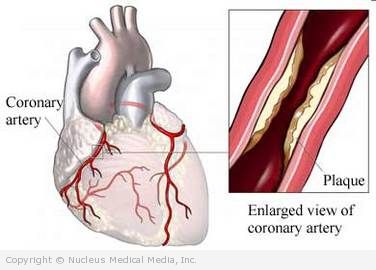
Angina is usually a sign of coronary artery disease (CAD). It occurs when the blood vessels leading to the heart are blocked. The blockage decreases the blood and oxygen flow to the heart muscle. When the heart muscle is deprived of oxygen, you will feel chest pain and other symptoms.
Stable or Unstable Angina
Angina occurs when your heart’s need for blood and oxygen is increased by:
- Exercise, exertion
- Cold weather
- A large meal
- Emotional stress
Stable angina becomes unstable when symptoms:
- Occur more often
- Last longer
- Are triggered more easily
Variant or Prinzmetal’s Angina
This type of angina is usually caused by a spasm of a heart vessel. It may indicate that you have one of the following conditions:
- CAD
- Extremely high blood pressure
- Hypertrophic cardiomyopathy
- Diseases of the heart valves
Angina – Risk Factors
Major risk factors for CAD include the following:
- Gender: male
- Increased age
- Strong family history of heart disease
- Obesity and overweight
- Smoking
- High blood pressure
- Sedentary lifestyle
- High blood cholesterol (specifically, high LDL cholesterol and low HDL cholesterol)
- Diabetes
Other risk factors for CAD:
- Stress
- Excessive alcohol intake
Angina – Symptoms
- Pressure or squeezing chest pain
- Some people do not experience the pain as severe
- Elderly people, women, and people with diabetes are more likely to have atypical or subtle symptoms
- Some people have silent ischemia (lack of blood supply to the heart) and experience no symptoms of chest pain
- Chest pain of any kind requires a medical evaluation to determine the cause
- Chest pain or discomfort is the key symptom of angina
The likelihood of a heart attack is increased when chest discomfort is severe, lasts more than 15 minutes, and is accompanied by other symptoms such as:
- Pain in the shoulder(s) or arm(s), or into the jaw
- Weakness
- Sweating
- Nausea
- Shortness of breath
Angina – Diagnosis
Tests will be done right away to see if you are having an episode of angina or a heart attack. If you have a stable pattern of angina, other tests may be done to determine the extent of your disease. The test results will help to create a treatment plan.
The doctor will ask about your symptoms and medical history. A physical exam will be done.
Tests may include:
- Blood tests
- Electrocardiogram (ECG, EKG)
- Echocardiogram
- Exercise stress test
- A medication is used to simulate the effects of physical exertion for those who can not exercise
- Nuclear scanning
- Electron-beam CT scan (coronary calcium scan, heart scan, CT angiography)
- American Heart Association (AHA) guidelines state that heart scans are not for everyone and are most likely to benefit patients at intermediate risk of CAD
- Coronary angiography
Angina – Treatment
Treatments for angina include:
Medications
- Nitroglycerin — usually given during an attack of angina as a tablet that dissolves under the tongue or as a spray
- Longer-lasting types may be used to prevent angina before an activity. May be given as pills, or applied as patches or ointments.
- Blood thinners — a small, daily dose of aspirin has been shown to decrease the risk of heart attack.
- Some may benefit from the addition of warfarin (Coumadin). There is an increased risk of bleeding with this drug.
- Talk to your doctor before taking aspirin daily or warfarin.
- Beta-blockers and calcium-channel blockers — may reduce the occurrence of angina
- Cholesterol-lowering medications — may prevent the progression of CAD; may even improve existing CAD
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) — lower blood pressure and decrease the workload on the heart
- Ranolazine (Ranexa) — to treat angina
Surgery
Patients with severe angina or unstable, progressing angina may benefit from:
- Coronary artery bypass graft — uses arteries from other areas of your body to bypass blocked heart arteries
- Coronary angioplasty — uses a balloon to open blocked arteries
Angina – Prevention
If you already have angina, you can prevent an onset by being aware of what starts it.
If you don’t have angina, preventing the development of CAD may reduce your chance of getting the condition.
Steps to prevent CAD include managing risk factors:
- Maintain a healthy weight.
- Begin a safe exercise program with the advice of your doctor.
- Stop smoking.
- Eat a healthy diet. It should be low in saturated fat. It should also be rich in whole grains, fruits, and vegetables.
- Appropriately treat high blood pressure and/or diabetes.
- Appropriately treat abnormal cholesterol levels or high triglycerides.